Book Appointment Now
Understanding Colon Cancer
Colon Cancer Guide
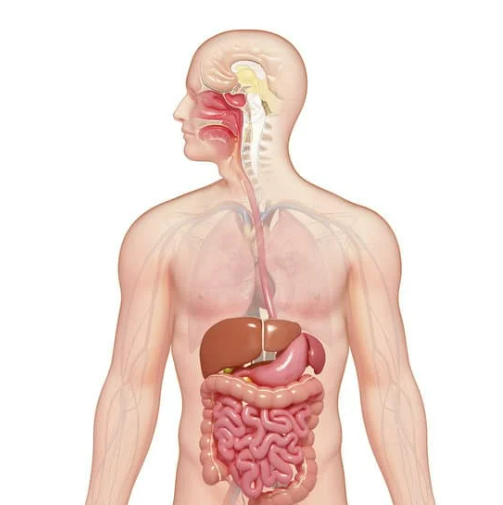
Introduction
Colon cancer, a type of colorectal cancer, arises from the inner lining of the large intestine. Historically, it has been a significant health concern due to its high incidence and mortality rates. Over the past few decades, advancements in medical research have led to a better understanding of its pathogenesis, risk factors, and treatment modalities. Recent developments emphasize the importance of early detection, personalized medicine, and lifestyle modifications in managing and preventing colon cancer. Studying this cancer is crucial as it remains one of the leading causes of cancer-related deaths worldwide, and understanding it can lead to improved outcomes and survival rates.
Statistics
Globally, colon cancer is the third most commonly diagnosed cancer and the second leading cause of cancer-related deaths. According to the World Health Organization, in 2020, approximately 1.9 million new cases were reported, with around 935,000 deaths attributed to colorectal cancers.
- Gender Disparities: Men have a slightly higher incidence rate than women.
- Age Factors: While traditionally affecting individuals over 50, there’s an alarming rise in cases among younger populations.
- Geographical Variations:
- High-Income Countries: Stabilizing or decreasing incidence due to effective screening programs.
- Low- and Middle-Income Countries: Increasing incidence attributed to westernized diets and lack of screening.
Key Statistics
- Lifetime Risk:
- Men: Approximately 1 in 23.
- Women: Approximately 1 in 25.
- 5-Year Survival Rates:
- Localized Stage: Over 90%.
- Regional Spread: Approximately 71%.
- Distant Metastasis: Around 14%.
- Trends Over Time:
- Decline in Mortality: Improved treatments and screening have reduced mortality rates by about 2% annually in high-income regions.
- Increase in Early-Onset Cases: Rising incidence among individuals under 50 years old.
Medical Illustrations
- Colon tumor:
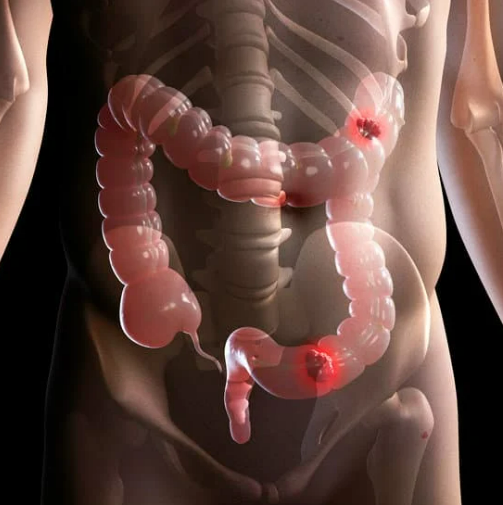
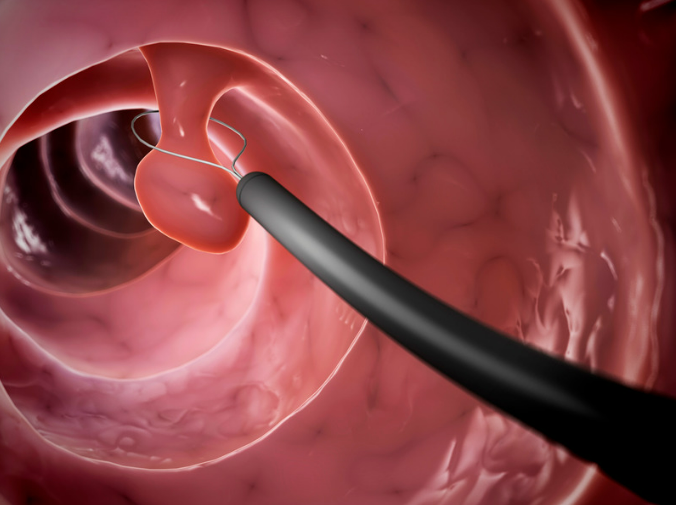
Colon polyp:
Risk Factors and Prevention
Known Risk Factors
Genetic Factors:
- Hereditary Syndromes:
- Lynch Syndrome: Increases lifetime risk significantly.
- Familial Adenomatous Polyposis (FAP): Leads to numerous polyps and early-onset cancer.
- Family History: First-degree relatives with colon cancer double one’s risk.
Environmental and Lifestyle Factors:
- Diet: High intake of red and processed meats linked to increased risk.
- Physical Inactivity: Sedentary lifestyle contributes to higher incidence.
- Obesity: Associated with increased risk and poorer outcomes.
- Smoking and Alcohol: Both are established risk factors.
- Inflammatory Bowel Disease: Conditions like ulcerative colitis elevate risk.
Recent meta-analyses reinforce these factors, highlighting the multifaceted nature of colon cancer risk.
Preventive Strategies
Lifestyle Modification:
- Dietary Changes: Emphasize fruits, vegetables, and whole grains.
- Regular Exercise: At least 150 minutes of moderate activity weekly.
- Weight Management: Maintaining a healthy BMI reduces risk.
Chemoprevention:
- Aspirin and NSAIDs: Long-term use linked to reduced polyp formation. A study in The Lancet (2018) showed a 24% reduction in incidence with regular aspirin use, but risks include gastrointestinal bleeding.
Screening and Surveillance:
- High-Risk Monitoring: More frequent screenings for those with genetic predispositions.
- Early Detection: Regular screenings starting at age 45 for average-risk individuals.
Screening
Current Screening Methods
| Method | Efficacy | Risks/Benefits | Cost Effectiveness |
|---|---|---|---|
| Colonoscopy | Gold standard; detects and removes polyps; sensitivity >95% for advanced lesions | Invasive; risks include perforation (~0.1%) and bleeding; requires sedation | High upfront cost but cost-effective long-term due to prevention |
| Fecal Immunochemical Test (FIT) | Non-invasive; detects occult blood; sensitivity ~79% for cancer | No procedural risks; must be done annually; less effective for detecting advanced adenomas | Low cost; increases screening compliance |
| CT Colonography | Less invasive; sensitivity ~90% for large polyps (>10mm) | Radiation exposure; cannot remove polyps during procedure; false positives may require follow-up colonoscopy | Moderate cost; alternative for those unable to undergo colonoscopy |
| Flexible Sigmoidoscopy | Examines lower colon; reduces mortality by detecting distal lesions | Misses proximal cancers; minimal risks; usually does not require sedation | Lower cost; less comprehensive |
Comparative studies indicate that while colonoscopy is most effective, FIT increases overall screening rates due to its non-invasive nature.
Symptoms and Signs
- Early Stages: Often asymptomatic; underscores the importance of routine screening.
- Intermediate Stages:
- Altered Bowel Habits: Diarrhea, constipation, or stool narrowing.
- Rectal Bleeding: Blood in stool or on toilet paper.
- Abdominal Discomfort: Cramps, gas, or persistent pain.
- Advanced Stages:
- Weakness and Fatigue: Due to anemia from chronic blood loss.
- Unexplained Weight Loss: Significant loss without dietary changes.
- Misdiagnoses and Atypical Presentations:
- Younger patients may be misdiagnosed with hemorrhoids or IBS.
- A clinical case highlighted a 35-year-old misdiagnosed for months due to age bias.
Diagnosis Steps
- Initial Assessment:
- Medical History: Evaluate symptoms and family history.
- Physical Examination: Check for abdominal masses or tenderness.
- Laboratory Tests:
- Complete Blood Count (CBC): Detects anemia.
- Liver Function Tests: Assesses potential liver metastasis.
- Colonoscopy:
- Procedure: Visual inspection and biopsy of suspicious areas.
- Imaging Studies:
- CT Scan: Evaluates abdominal and pelvic regions for spread.
- MRI: Detailed imaging, especially for rectal cancer staging.
- Pathological Examination:
- Biopsy Analysis: Confirms cancer type and grade.
- Tumor Marker Testing:
- Carcinoembryonic Antigen (CEA): Baseline level for monitoring treatment response.
Stages
Types of Treatment
Surgery:
- Purpose: Remove the tumor and regional lymph nodes.
- Procedures:
- Colectomy: Partial or total removal of the colon.
- Laparoscopic Surgery: Minimally invasive option.
- Side Effects: Infection, bleeding, changes in bowel habits.
Radiation Therapy:
- Usage: Primarily for rectal cancer; pre- or post-operative.
- Side Effects: Skin irritation, fatigue, bowel discomfort.
Chemotherapy:
- Common Regimens: FOLFOX (5-FU, leucovorin, oxaliplatin).
- Mechanism: Inhibits DNA synthesis in rapidly dividing cells.
- Side Effects: Nausea, hair loss, neuropathy.
Immunotherapy:
- Agents: Pembrolizumab for MSI-H tumors.
- Mechanism: Enhances the immune system’s ability to fight cancer.
- Side Effects: Immune-mediated reactions like colitis.
Evidence-Based Comparisons
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Chemotherapy | Inhibits cell division (e.g., 5-FU) | Hair loss, nausea, neuropathy | ~50% 5-year survival in stage III | MOSAIC Trial (2004) |
| Immunotherapy | Boosts immune response (PD-1 inhibitors) | Fatigue, rash, colitis | Improved OS in MSI-H tumors | KEYNOTE 177 (2020) |
| Chemotherapy | Inhibits cell division (e.g., 5-FU) | Hair loss, nausea, neuropathy | ~50% 5-year survival in stage III | MOSAIC Trial (2004) |
MOSAIC Trial (2004): Demonstrated the efficacy of adding oxaliplatin to 5-FU, improving disease-free survival.
KEYNOTE-177 (2020): Showed pembrolizumab improved progression-free survival compared to chemotherapy in MSI-H metastatic colorectal cancer.
Additional Resources
- Patient Advocacy Groups:
- Key Opinion Leaders:
- Dr. Bert Vogelstein: Pioneer in genetic research of colon cancer.
- Clinical Trials:
- ClinicalTrials.gov: Database for ongoing research studies.
- The Cancer Genome Atlas (TCGA): Comprehensive genomic data.
Key Findings
- Screening Saves Lives: Early detection through screening significantly reduces mortality.
- Lifestyle Matters: Diet and exercise are modifiable risk factors that can lower risk.
- Advancements in Treatment: Personalized medicine and immunotherapies have improved outcomes.
- Rising Early-Onset Incidence: Highlights the need for increased awareness and potentially earlier screening.
- Health Disparities Exist: Socioeconomic factors affect access to care and outcomes.
Discussion
The declining mortality rates in high-income countries underscore the success of screening programs and advanced treatments. However, the rising incidence among younger individuals is concerning and suggests environmental and lifestyle factors play a significant role. Disparities in outcomes highlight the need for equitable access to screening and care.
While colonoscopy remains the gold standard for screening, non-invasive methods like FIT have improved participation rates. Treatment advances, particularly in immunotherapy for MSI-H tumors, offer hope but are applicable to a subset of patients. Ongoing research into biomarkers and genetic profiling is crucial for developing targeted therapies.
Final Recommendations
- Clinical Recommendations:
- Initiate screening at age 45 for average-risk individuals.
- Employ genetic testing for high-risk patients to guide treatment.
- Encourage lifestyle modifications as part of preventive care.
- Research Directions:
- Investigate causes of early-onset colon cancer.
- Develop non-invasive screening tools with higher sensitivity.
- Explore combination therapies to improve efficacy.
- Policy Suggestions:
- Implement public health campaigns targeting awareness in younger populations.
- Ensure accessibility and affordability of screening and treatments across all demographics.
- Fund research focusing on health disparities to improve outcomes for underserved communities.
Disclaimer
This article reflects current knowledge as of October 2023. Medical research is continually evolving, and newer information may emerge. This content is for informational purposes and should not substitute professional medical advice. Always consult healthcare professionals for personal medical guidance.
