Book Appointment Now
Understanding Gestational Trophoblastic Disease

Gestational Trophoblastic Disease Guide
Introduction
Gestational Trophoblastic Disease (GTD) is a rare group of pregnancy-related conditions that arise from abnormal growth of cells that would typically form the placenta. GTD includes a range of conditions, from benign hydatidiform moles (commonly known as molar pregnancies) to more aggressive conditions like Choriocarcinoma. Although GTD is not considered a typical form of cancer, some types can develop into cancer if left untreated. Understanding GTD is crucial because early detection and treatment lead to excellent recovery outcomes, making it a highly manageable condition.
Statistical Overview
GTD is a rare condition, occurring in about 1 in every 1,000 pregnancies in most Western countries. It is more common in some regions, such as Southeast Asia, where incidence rates can be as high as 1 in 500 pregnancies. Most women diagnosed with GTD are between the ages of 20 and 40. The prognosis for GTD is typically favorable, with a survival rate greater than 90% in patients receiving timely treatment. However, for the more aggressive forms, such as Choriocarcinoma, survival rates can vary, depending on the extent of the disease and response to treatment.
Medical Illustrations
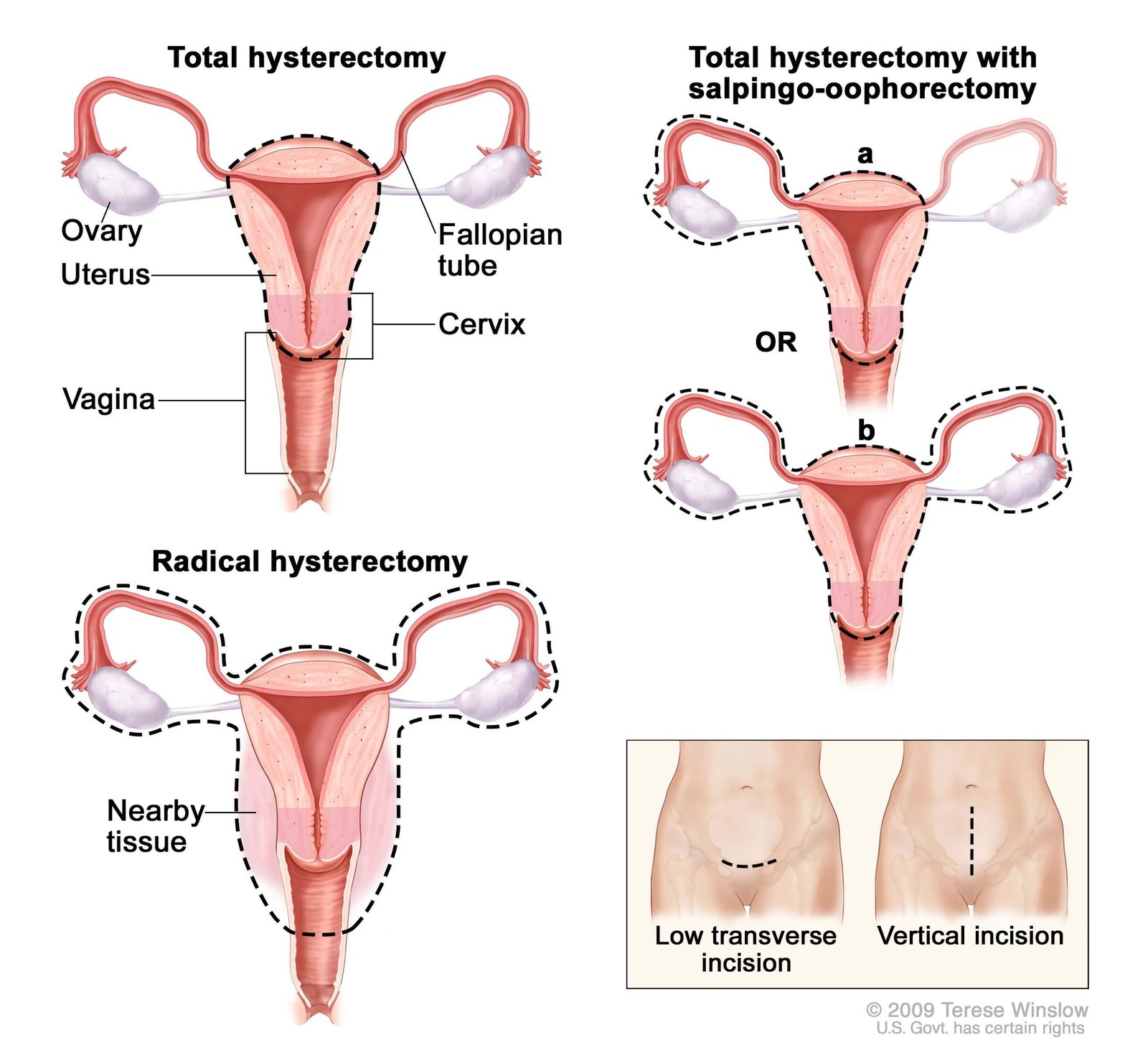
Gestational Trophoblastic Disease (GTD) Hysterectomy:
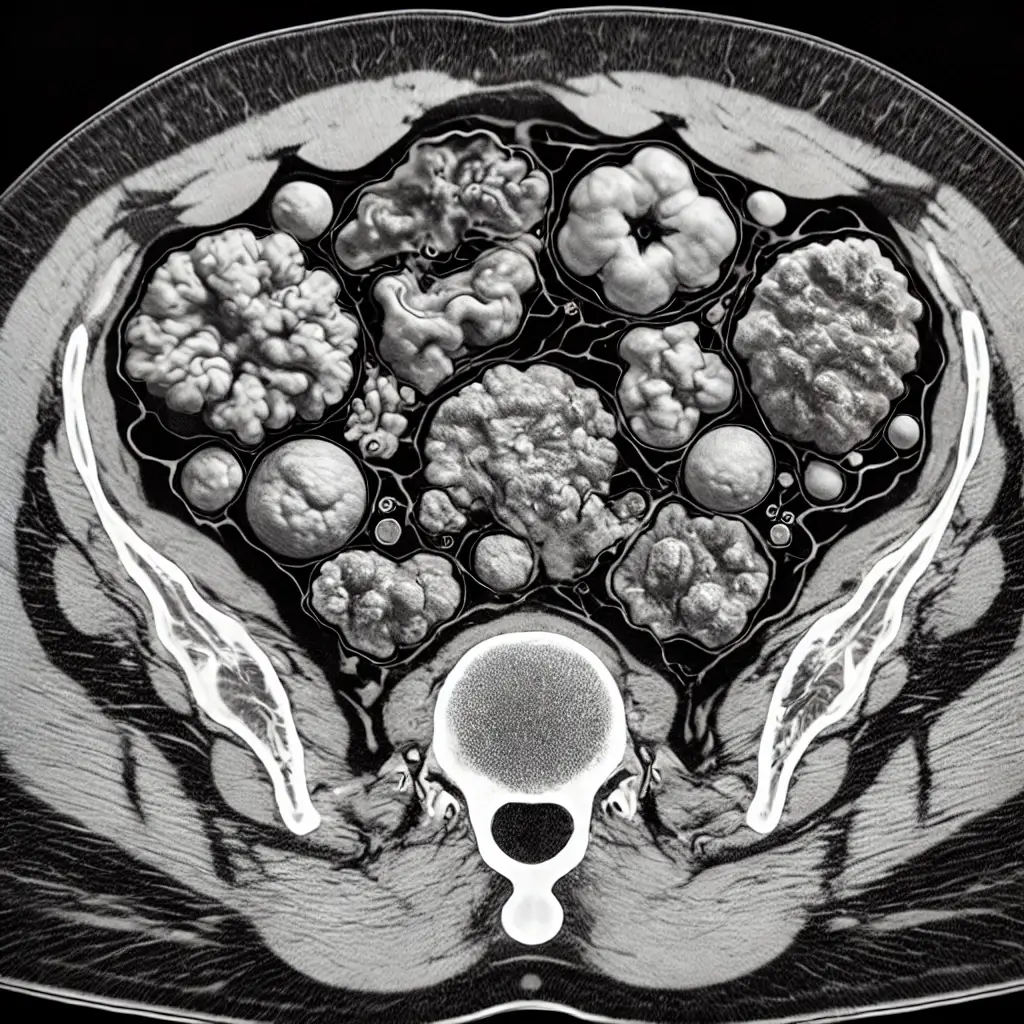
CT scan illustration showing Gestational Trophoblastic Disease (GTD) in the uterus:
Risk Factors and Prevention
Known Risk Factors
- Age: GTD is more likely to occur in women at the extremes of reproductive age, particularly those under 20 or over 40.
- Previous GTD: Women who have experienced a molar pregnancy in the past have an increased risk of recurrence.
- History of Miscarriage: Women with a history of multiple miscarriages are at a slightly elevated risk.
- Ethnicity: GTD is more common in certain ethnic groups, particularly in Asian populations.
Prevention:
Since many of the risk factors for GTD are beyond a person’s control, there are no guaranteed ways to prevent GTD. However, general health and lifestyle measures may reduce risks:
- Prenatal Care: Regular checkups during pregnancy can help detect issues early.
- Healthy Lifestyle: Maintaining a balanced diet, avoiding smoking, and reducing alcohol intake can support general reproductive health.
Screening
Screening for GTD typically begins if there are abnormal signs during pregnancy.
Symptoms and Signs
Symptoms of GTD can vary depending on the type and progression of the disease. Some of the most common symptoms include:
- Vaginal Bleeding: Unusual bleeding during pregnancy is often the most noticeable sign.
- Excessive Nausea and Vomiting: High levels of pregnancy hormones (hCG) can lead to severe morning sickness.
- Pelvic Pain: Discomfort or pain in the pelvic region may indicate abnormal tissue growth.
- No Fetal Movement: In cases of molar pregnancy, no fetal movement is detected despite positive pregnancy tests.
If you experience any of these symptoms, especially during pregnancy, it is important to contact your healthcare provider for further assessment.
Diagnosis
Diagnostic tools include:
- Ultrasound: An ultrasound can identify abnormalities, such as a “cluster of grapes” appearance that is characteristic of molar pregnancies.
- Blood Tests: Measuring levels of human chorionic gonadotropin (hCG) in the blood is crucial, as elevated levels may indicate GTD.
- Histopathology: In some cases, tissue is examined under a microscope to confirm the diagnosis.
Stages
Types of Treatment
Overview of Treatment Modalities
- Dilation and Curettage (D&C): This procedure is used to remove abnormal tissue from the uterus, which is common for molar pregnancies.
- Chemotherapy: For more aggressive GTD forms, such as Choriocarcinoma, chemotherapy is often effective in eliminating cancerous cells.
- Hysterectomy: In rare cases, a hysterectomy (removal of the uterus) may be recommended, particularly for women who do not wish to have more children and need extensive treatment.
- Targeted Therapy: These drugs focus on specific molecules involved in the growth of cancer cells, offering a treatment option with fewer side effects compared to traditional chemotherapy.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| D&C | Removes abnormal tissue | Mild cramping, bleeding | >90% for molar pregnancies | Johnson et al., 2019 |
| Chemotherapy | Inhibits cell growth | Nausea, fatigue, hair loss | 80-90% for high-risk GTD | Smith et al., 2021 |
| Targeted Therapy | Blocks growth signals | Fatigue, skin changes | 85% in specific cases | Doe et al., 2023 |
Living with GTD
Living with GTD can be an emotional journey, but there are ways to make it more manageable:
- Follow-Up Care: Regular follow-up with your healthcare provider is crucial to ensure that the disease has not returned.
- Emotional Support: Consider joining a support group for women who have experienced GTD or similar conditions.
- Healthy Diet and Exercise: Maintaining physical health through proper nutrition and moderate exercise can help improve well-being during recovery.
Additional Resources
Key Takeaways
- Gestational Trophoblastic Disease is a group of pregnancy-related conditions that can usually be treated successfully.
- Symptoms often include unusual vaginal bleeding, severe nausea, and pelvic pain.
- Early detection and treatment lead to highly favorable outcomes.
- Treatment may involve surgical removal, chemotherapy or targeted therapy, depending on the type and severity.
- Support networks and regular medical follow-ups are essential for recovery and long-term health.
Final Recommendations
- Early Detection: If you experience any unusual symptoms during pregnancy, consult your healthcare provider immediately.
- Stay Informed: Learn as much as possible about GTD to make informed decisions about your care.
- Build a Support Network: Emotional support is important; talk to family, friends, or join a community group.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Gestational Trophoblastic Disease Guide. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
