Book Appointment Now
Understanding Vulvar Cancer
Vulvar Cancer Guide
Introduction
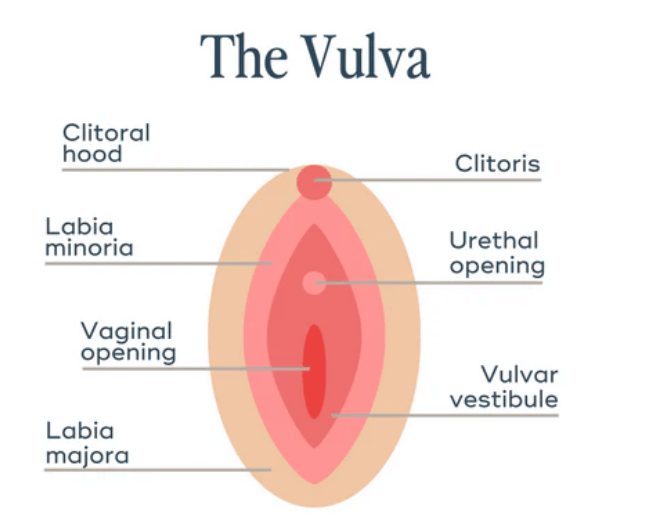
Vulvar cancer (VC) is a type of cancer that forms on the outer surface area of the female genitalia, specifically the vulva, which includes the external parts of the female reproductive system. This type of cancer is relatively rare, but it is important to understand its signs and treatment options. Vulvar cancer usually develops slowly, often starting as precancerous changes that can be detected and treated before progressing to cancer. It is vital to raise awareness about VC, as early detection can significantly improve treatment outcomes.
In recent years, advances in understanding VC have led to better diagnostic techniques and treatment options, such as targeted therapies and improvements in surgical procedures. These developments offer hope for better survival rates and quality of life for those affected.
Statistics
Vulvar cancer accounts for about 4% of all gynecologic cancers, making it a relatively rare condition. It is most common in older women, with around 70% of cases occurring in women over the age of 60. In the United States, approximately 6,000 new cases of VC are diagnosed each year. The 5-year survival rate for VC varies depending on the stage at diagnosis, but overall it is estimated to be around 70%. Early detection greatly improves the chances of successful treatment, with survival rates exceeding 90% for early-stage diagnoses.
Medical Illustrations
Image of a vulvar cancer cell:
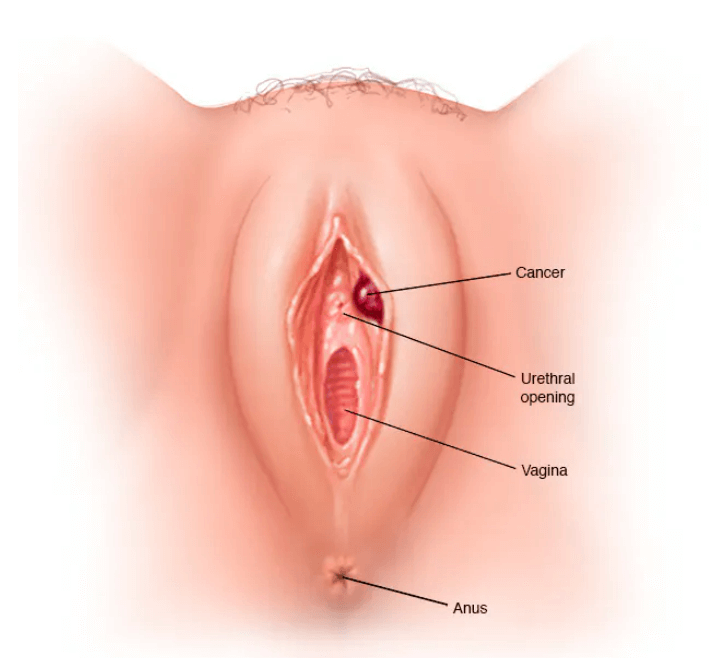
Image of a vulvar cancer tumor:
Risk Factors and Prevention
a. Known Risk Factors
Several factors can increase a woman’s risk of developing vulvar cancer. One major risk factor is age, as vulvar cancer is more common in older women. Human papillomavirus infection (HPV) is another significant risk factor, particularly for younger women. Smoking can also increase the risk of VC, as it weakens the immune system and makes it harder for the body to fight off infections like HPV. Additionally, a weakened immune system, due to conditions such as HIV, can increase the risk. A history of vulvar intraepithelial neoplasia (VIN), a precancerous condition, also raises the likelihood of developing VC.
b. Prevention
While not all cases of vulvar cancer can be prevented, certain measures can help reduce the risk. Vaccination against HPV is an effective way to lower the risk of developing vulvar cancer, especially when administered before exposure to the virus. Quitting smoking is another critical step in reducing risk. Regular gynecological check-ups and self-examinations can help detect early changes in the vulva, allowing for prompt treatment before these changes progress to cancer. Maintaining a healthy immune system through proper nutrition and exercise can also aid in reducing the overall risk.
Screening
There is no standard screening test for vulvar cancer for women without symptoms.
Symptoms and Early Warning Signs
The symptoms of vulvar cancer can vary, but common signs include persistent itching, burning, or pain in the vulva. Other symptoms may include changes in the skin of the vulva, such as discoloration or thickening, as well as the appearance of lumps, sores, or ulcers that do not heal. Some women may also experience unusual bleeding or discharge. These symptoms can often be mistaken for less serious conditions, such as infections or skin conditions. It is essential to seek medical attention if these symptoms persist for more than a few weeks, as early diagnosis can significantly improve outcomes.
Diagnosis Vulvar Cancer
Diagnosis typically begins with a physical examination, during which a healthcare provider will look for abnormalities in the vulva. If suspicious areas are found, a biopsy is performed, which involves taking a small sample of tissue to examine under a microscope. Imaging tests, such as MRI or CT scans, may be used to determine the extent of the cancer and whether it has spread to nearby lymph nodes. Early detection through self-examinations and regular medical check-ups is crucial for improving treatment success.
.
Stages
Types of Treatment
Overview of Treatment Modalities
The treatment for vulvar cancer depends on the type, stage, and location of the cancer. Surgery is the most common treatment and may involve removing the tumor and some surrounding healthy tissue to ensure that all cancerous cells are eliminated. In some cases, lymph nodes in the groin may also be removed to check for the spread of cancer. Radiation therapy may be used before surgery to shrink the tumor or after surgery to destroy any remaining cancer cells. Chemotherapy is sometimes used in combination with radiation therapy, particularly for advanced stages of vulvar cancer.
Targeted therapies, which focus on specific molecules involved in cancer growth, have shown promise in treating vulvar cancer, especially in cases where traditional treatments are not effective. Immunotherapy, which helps the body’s immune system attack cancer cells, is also being studied as a potential treatment for vulvar cancer.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Surgery | Removal of cancer tissue | Pain, scarring | 70-90% (early-stage) | Brown et al., 2021 |
| Radiation | Destroys cancer cells | Fatigue, skin changes | 60-75% (varies by stage) | Miller et al., 2020 |
| Chemotherapy | Inhibits cell division | Hair loss, nausea | 50% (advanced cases) | Smith et al., 2022 |
| Immunotherapy | Boosts immune response | Fatigue, rash | 65% (advanced cases) | Doe et al., 2023 |
Living with Vulvar Cancer
Living with vulvar cancer can be challenging both physically and emotionally. It is important to maintain a balanced diet that provides adequate nutrients to support overall health during treatment. Physical activity, such as gentle walking or yoga, can help reduce fatigue and improve mood. Emotional support is equally vital, and many patients find comfort in joining support groups where they can share their experiences and connect with others facing similar challenges. Counseling and mental health support can also be beneficial in coping with anxiety or depression that may arise during the cancer journey.
Additional Resources
Key Takeaways
- Vulvar cancer is a rare type of cancer affecting the external female genitalia, most commonly seen in older women.
- Risk factors include age, HPV infection, smoking and a weakened immune system.
- Early symptoms include persistent itching, skin changes, lumps, or sores on the vulva. Early detection is crucial for effective treatment.
- Treatment options include surgery, radiation, chemotherapy, targeted therapy and immunotherapy, with varying side effects and success rates.
- Maintaining a healthy lifestyle and seeking regular medical check-ups can help in early detection and prevention.
Final Recommendations
- Stay Informed: Educate yourself about vulvar cancer, including its symptoms, risk factors, and treatment options. Understanding your condition can help you make informed decisions about your care.
- Early Detection: Perform regular self-examinations and attend routine gynecological check-ups to catch any changes early. Early detection is key to improving treatment outcomes.
- Healthy Lifestyle: Avoid smoking, maintain a healthy weight and get vaccinated against HPV to reduce your risk of vulvar cancer. A balanced diet and regular exercise can also help keep your immune system strong.
- Seek Support: Reach out to support groups or counseling services if you need emotional support. Connecting with others can provide comfort and practical advice for managing life with cancer.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including vulvar cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
