Book Appointment Now
Understanding Malignant Peritoneal Mesothelioma
Malignant Peritoneal Mesothelioma Guide
Introduction
Introduction
Malignant peritoneal mesothelioma (MPM) is a rare and aggressive cancer that forms in the peritoneum, the thin layer of tissue lining the abdomen. This cancer is strongly linked to asbestos exposure and accounts for a small percentage of all mesothelioma cases. Although rare, advances in treatment strategies, including cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC), have improved survival rates and quality of life for many patients. Early detection remains a challenge due to its nonspecific symptoms.
Statistics
Peritoneal mesothelioma represents about 20% of all mesothelioma cases, with an estimated 500-600 new cases annually in the United States. The disease often affects individuals over 50, with a slight male predominance. The median survival rate has increased to 53 months in patients undergoing aggressive treatment, compared to 6-12 months in untreated cases.
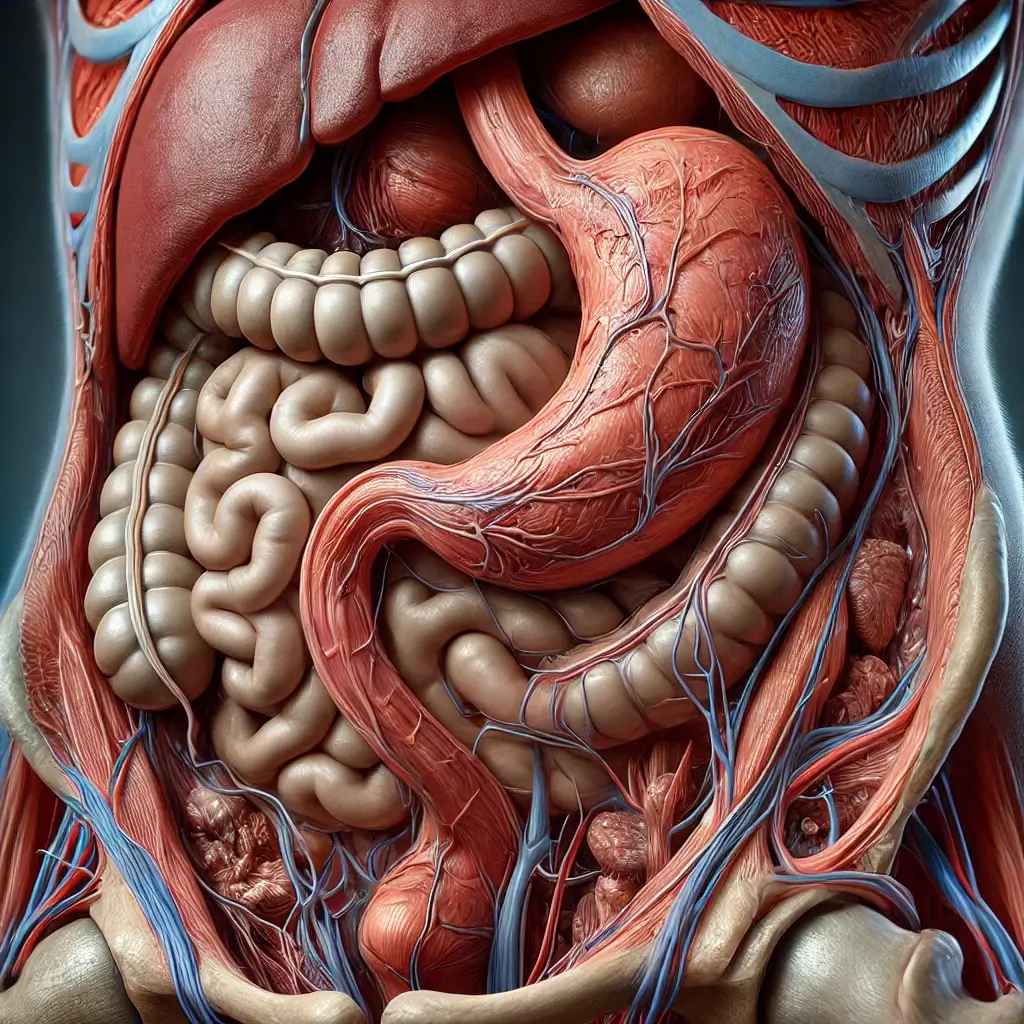
Medical Illustrations
A highly detailed close-up view of an asbestos-containing surface:

Histological section of Malignant Peritoneal Mesothelioma under a microscope:

Risk Factors and Prevention
a. Known Risk Factors
The primary risk factor for malignant peritoneal mesothelioma is asbestos exposure. Other contributing factors include:
- Occupational Exposure: Jobs in construction, shipbuilding and mining often involve asbestos exposure.
- Environmental Exposure: Living near asbestos-contaminated sites increases risk.
- Genetic Susceptibility: Mutations in the BAP1 gene may predispose individuals to mesothelioma.
- Radiation Therapy: Previous radiation treatments to the abdomen may elevate risk.
b. Prevention
- Avoid exposure to asbestos by using protective gear in high-risk occupations.
- Adhere to safety regulations for asbestos removal and handling.
- Regular health screenings for individuals with known asbestos exposure.
Screening
Symptoms and Early Warning Signs
MPM symptoms often overlap with other abdominal conditions, leading to delayed diagnosis. Common signs include:
- Abdominal pain or swelling
- Unexplained weight loss
- Loss of appetite
- Nausea or vomiting
- Changes in bowel habits (diarrhea or constipation)
- Fatigue
- Fluid buildup in the abdomen (ascites)
If symptoms persist or worsen, especially in individuals with asbestos exposure, seek medical evaluation promptly.
Diagnosis
Diagnosing peritoneal mesothelioma involves a combination of clinical evaluation and advanced diagnostic tools:
- Physical Examination: Focuses on detecting abdominal masses or ascites.
- Imaging Tests: CT scans and MRIs provide detailed views of the abdomen to identify tumors and assess disease extent.
- Biopsy: A tissue sample is obtained through laparoscopic surgery to confirm the diagnosis.
- Blood Tests: Biomarkers like mesothelin-related proteins may aid in diagnosis.
- Genetic Testing: Identifies mutations, such as in the BAP1 gene, which can guide treatment planning.
Stages
Types of Treatment
Overview of Treatment Modalities
A multidisciplinary approach combining surgery, chemotherapy and emerging therapies offers the best outcomes for MPM patients. Treatment options include:
- Cytoreductive Surgery (CRS):
- Removes visible tumors in the abdomen and is often combined with HIPEC.
- Hyperthermic Intraperitoneal Chemotherapy (HIPEC):
- Delivers heated chemotherapy directly into the abdominal cavity post-surgery, targeting residual cancer cells.
- Systemic Chemotherapy:
- Administers chemotherapy through the bloodstream for advanced or inoperable cases.
- Immunotherapy:
- Uses immune checkpoint inhibitors to boost the body’s ability to target cancer cells.
- Clinical Trials:
- Investigate novel therapies, such as targeted therapies and combination treatments.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| CRS + HIPEC | Removes and targets residual tumors | Pain, infection | Median survival 53 months | Sugarbaker et al., 2022 |
| Systemic Chemotherapy | Inhibits cell division | Nausea, fatigue | Median survival 12-18 months | Lee et al., 2020 |
| Immunotherapy | Boosts immune response | Rash, flu-like symptoms | Promising for advanced cases | Carter et al., 2023 |
Living with MPM
Managing life with peritoneal mesothelioma involves addressing physical, emotional and practical challenges. Recommendations include:
- Nutritional Support: Work with a dietitian to manage treatment-related side effects and maintain strength.
- Pain Management: Consult specialists to develop an effective pain relief plan.
- Physical Activity: Engage in light exercises to reduce fatigue and improve overall well-being.
- Mental Health Care: Seek counseling or join support groups to manage emotional stress.
- Regular Follow-Ups: Essential for monitoring recurrence and adjusting treatment plans.
Additional Resources
Key Takeaways
- Malignant peritoneal mesothelioma is rare, but strongly linked to asbestos exposure.
- Symptoms like abdominal swelling, pain and ascites warrant immediate medical attention.
- CRS combined with HIPEC is the most effective treatment for eligible patients.
- Comprehensive care, including supportive therapies, improves survival and quality of life.
Final Recommendations
- Individuals with known asbestos exposure should remain vigilant for symptoms and seek regular health screenings.
- Discuss all treatment options, including participation in clinical trials, with a specialized care team.
- Focus on supportive care to enhance quality of life during and after treatment.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Malignant Peritoneal Mesothelioma (MPM). Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
