Book Appointment Now
Understanding Vaginal Cancer
Vaginal Cancer Guide
Introduction
Vaginal cancer is a rare malignancy originating in the tissues of the vagina, the muscular canal connecting the cervix to the outside of the body. Although it represents a small percentage of all gynecologic cancers, early detection is crucial for improving outcomes and quality of life. Often diagnosed incidentally during routine gynecological exams, vaginal cancer can be effectively managed, if caught in the early stages.
Statistics
- Vaginal cancer accounts for 1-2% of all gynecological cancers.
- In the United States, approximately 4,000 new cases are diagnosed each year.
- The most common histological type is squamous cell carcinoma, followed by adenocarcinoma.
- The five-year survival rate is around 84% for localized cases but drops significantly for advanced disease.
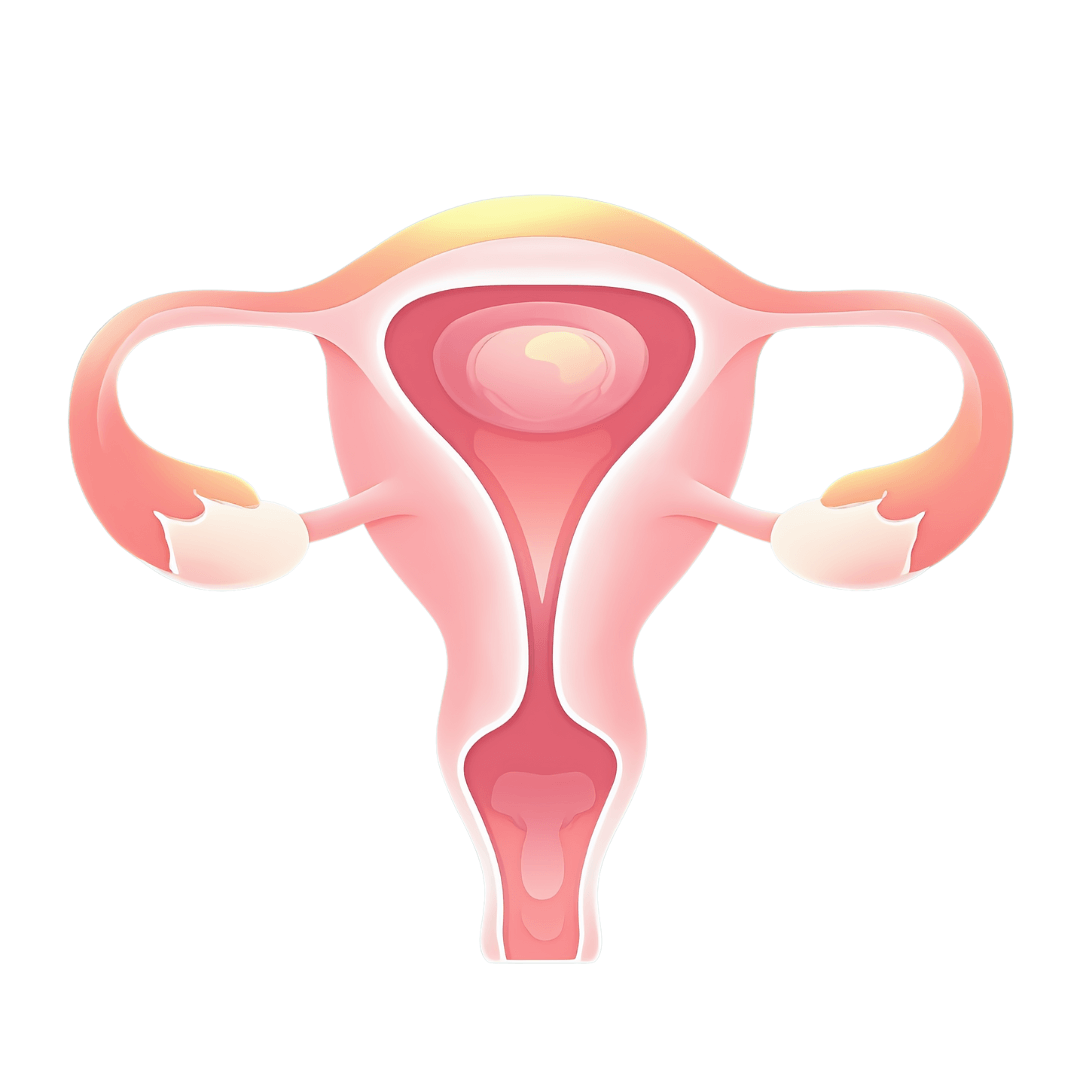
Medical Illustrations
MRI scan of female pelvis showing a visible mass within the vaginal canal – hypointense irregular lesion pressing against surrounding tissues:

View of squamous cell carcinoma of the vagina – irregular, hyperchromatic epithelial cells with keratin pearls and atypical mitotic figures:

Risk Factors and Prevention
a. Known Risk Factors
Several factors are associated with an increased likelihood of developing vaginal cancer:
- Human Papillomavirus (HPV): High-risk strains (e.g., HPV-16, HPV-18) are strongly linked to vaginal carcinoma.
- Age: Most cases occur in women over 60.
- History of Cervical Cancer: Previous cancer in the cervix raises the risk of vaginal malignancies.
- Vaginal Intraepithelial Neoplasia (VAIN): A precancerous lesion that can progress to invasive cancer.
- Diethylstilbestrol (DES) Exposure: Women exposed to DES in utero face a higher risk of clear cell adenocarcinoma.
- Smoking: Tobacco weakens the immune system and heightens susceptibility to cancers.
- Immunosuppression: Conditions like HIV/AIDS or immunosuppressive therapies elevate risk.
b. Prevention
- HPV Vaccination: Protects against oncogenic HPV strains.
- Regular Gynecological Exams: Pap tests and HPV testing enable early detection of precancerous changes.
- Lifestyle Modifications: Avoid smoking and maintain a robust immune system.
- Prompt Treatment of VAIN: Addressing precancerous changes early can prevent progression.
Screening
While there is no dedicated screening program exclusively for vaginal cancer, many cases are identified via routine gynecological exams. Key screening methods include:
- Pap Test and HPV Testing: Identifies precancerous or dysplastic changes.
- Colposcopy: Offers a magnified examination of the vaginal and cervical tissues.
- Biopsy: Confirms malignancy if suspicious lesions are detected.
Symptoms and Early Warning Signs
Symptoms may be nonspecific or overlap with other gynecologic issues. Common indicators are:
- Unusual vaginal bleeding, especially post-coital or post-menopausal.
- Watery or foul-smelling discharge.
- Dyspareunia (pain during intercourse).
- Palpable lump or mass in the vaginal canal.
- Pelvic discomfort or pain.
- Urinary frequency or difficulty emptying the bladder.
If such symptoms persist, a prompt medical evaluation is essential.
Diagnosis
Diagnosis involves multiple steps to accurately stage and classify the cancer:
- Pelvic Examination: Detects masses or irregularities.
- Pap and HPV Tests: Screen for dysplastic lesions and HPV status.
- Colposcopy: Visualizes abnormal areas needing biopsy.
- Biopsy: Confirms malignancy and determines cell type.
- Imaging Studies: CT, MRI, or PET scans assess tumor extent and potential metastases.
Stages
Types of Treatment
Overview of Treatment Modalities
Treatment depends on tumor histology, stage, and the patient’s overall health:
- Surgery
- Local Excision: Removes a small tumor and a margin of healthy tissue.
- Vaginectomy: Partial or total removal of the vagina, sometimes followed by reconstructive procedures.
- Radiation Therapy
- External Beam Radiation: Targets tumors externally.
- Brachytherapy: Delivers radiation internally for localized disease.
- Chemotherapy
- Often used with radiotherapy for advanced or recurrent cancers.
- Immunotherapy
- Newer approach boosting the immune response to cancer cells.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Surgery | Removes tumor | Pain, infection | 84% for localized cases | Smith et al., 2021 |
| Radiation Therapy | Shrinks or eliminates tumors | Fatigue, skin irritation | Effective for local control | Lee et al., 2020 |
| Chemotherapy | Targets rapidly dividing cells | Nausea, fatigue | Moderate for advanced stages | Carter et al., 2023 |
| Immunotherapy | Boosts immune response | Rash, flu-like symptoms | Promising in clinical trials | Brown et al., 2022 |
Living with Cancer
Coping with vaginal cancer requires addressing both physical and emotional challenges:
- Emotional Support: Consider therapy or support groups specialized in gynecologic cancers.
- Rehabilitation: Pelvic floor exercises and physiotherapy to restore function.
- Nutrition: A balanced diet aids in recovery and minimizes treatment side effects.
- Follow-Up Care: Regular check-ups detect recurrence or manage late side effects.
Additional Resources
Key Takeaways
- Vaginal cancer is uncommon, but early detection via screening is key.
- HPV infection is a major risk factor; vaccination and Pap/HPV testing are preventative measures.
- Treatment includes surgery, radiotherapy, chemotherapy, or immunotherapy, depending on stage and cell type.
- Ongoing support—physical, emotional, and social—is critical for a better quality of life.
Final Recommendations
- Stay informed about risk factors like HPV and discuss vaccination with a healthcare professional.
- Attend regular gynecological screenings to catch precancerous or early-stage lesions.
- Explore all treatment options, including clinical trials, if diagnosed.
- Utilize supportive care services (nutritionists, therapists, support groups) for comprehensive well-being.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Vaginal Cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
