Book Appointment Now
Understanding Adrenal Cancer
Adrenal Cancer Guide
Introduction
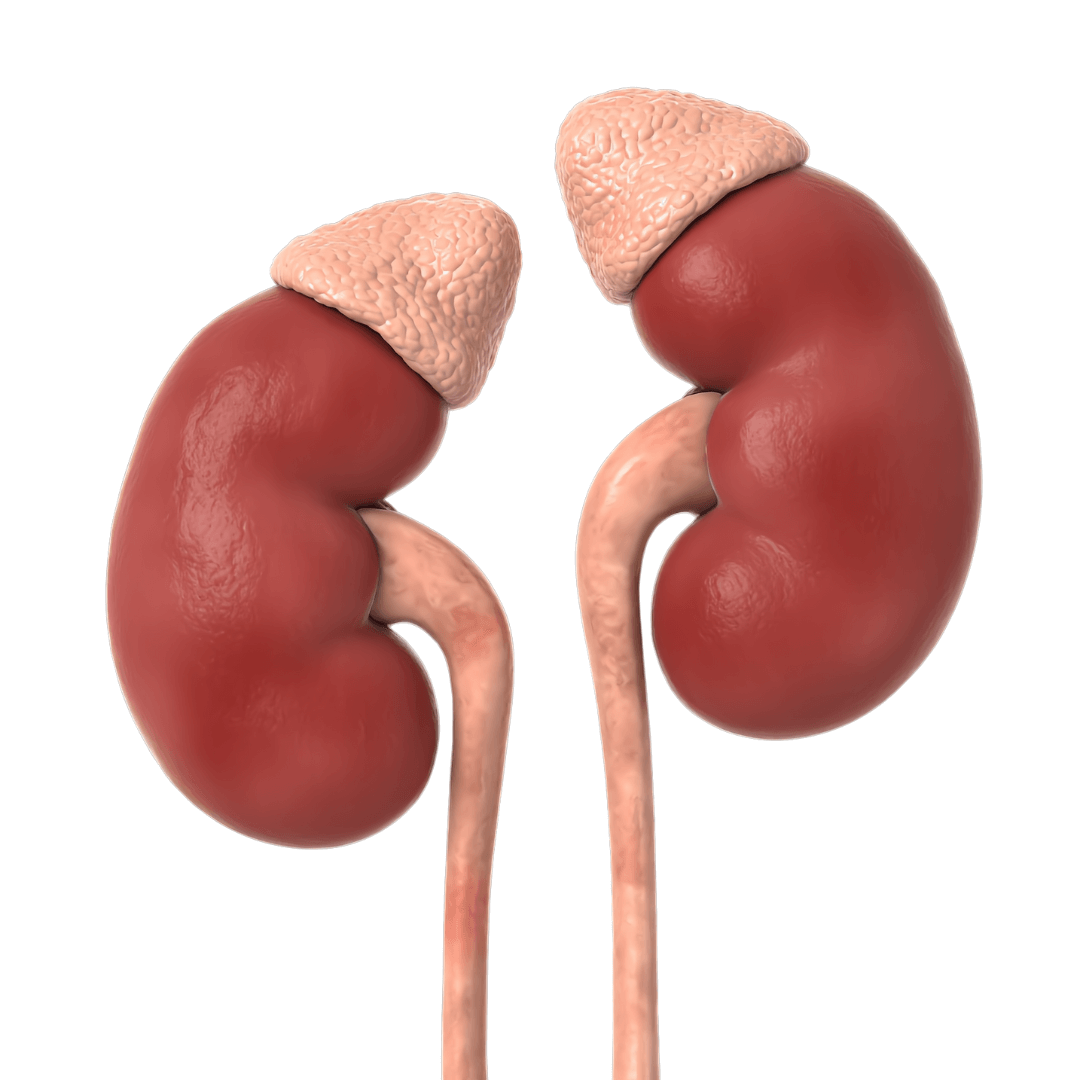
Adrenal cancer, also referred to as adrenocortical carcinoma (ACC), is a rare and aggressive malignancy originating in the adrenal glands. These small, triangular glands sit on the top of each kidney and play a vital role in hormone production. Due to its rarity and often non-specific symptoms, early detection is challenging. However, understanding risk factors and new treatment strategies can significantly improve outcomes.
Statistics
- Adrenal cancer accounts for approximately 0.02% of all cancers, with an incidence of 1-2 cases per million people each year.
- While it can occur at any age, it is most frequently diagnosed in adults aged 40-50 and in children under 5.
- The five-year survival rate is roughly 50-60% for localized disease, but decreases significantly for advanced stages.
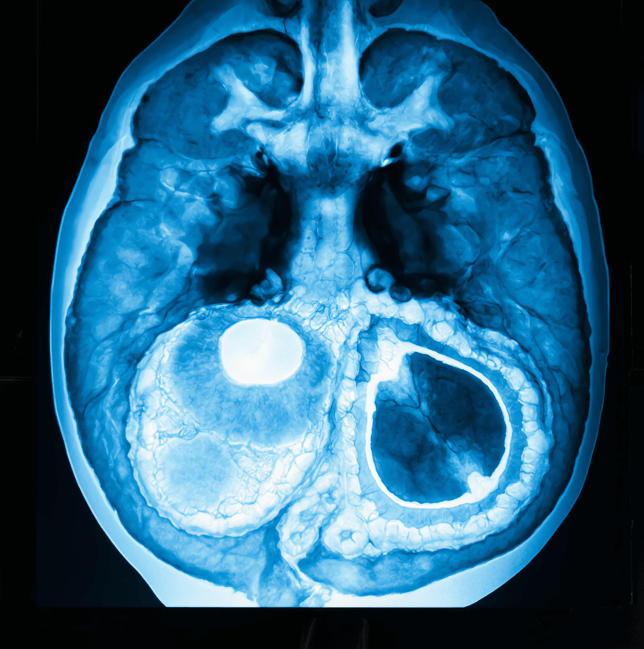
Medical Illustrations
Microscopic image of adrenocortical carcinoma – large polygonal cells with abundant eosinophilic cytoplasm:

CT scan of the upper abdomen showing a large adrenal mass on top of the right kidney – irregular, enhancing soft tissue lesion:
Risk Factors and Prevention
a. Known Risk Factors
- Genetic Syndromes: Conditions like Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome, and multiple endocrine neoplasia (MEN) type 1.
- Family History: A history of adrenal or other endocrine cancers.
- Hormonal Disorders: Excessive hormone production in the adrenal glands.
- Age and Gender: Slightly more common in women, often diagnosed in middle age.
b. Prevention
- Genetic Counseling and Testing: Particularly for individuals with a family history of hereditary cancer syndromes.
- Regular Medical Checkups: For early detection of hormonal imbalances or adrenal abnormalities.
Screening
No standardized screening program exists for adrenal cancer due to its low incidence. However, those at higher risk (e.g., with genetic predispositions) should undergo regular checkups, including:
- Imaging Studies (ultrasound, CT, or MRI), if clinically indicated.
- Blood and Urine Tests to detect abnormal hormone levels early.
Symptoms and Early Warning Signs
Symptoms vary based on whether the tumor is functional (producing hormones) or non-functional:
- Hormonal Symptoms:
- Excess Cortisol (Cushing’s Syndrome): Weight gain, high blood pressure, muscle weakness.
- Excess Aldosterone: Hypertension and low potassium levels.
- Excess Androgens or Estrogens: Abnormal hair growth or changes in secondary sexual characteristics.
- Non-Hormonal Symptoms:
- Abdominal Pain or Fullness
- Unexplained Weight Loss
- Palpable Abdominal Mass
Persistent or worsening symptoms warrant prompt medical evaluation.
Diagnosis Adrenal Cancer
Diagnosis relies on clinical assessments and specialized tests:
Biopsy: Occasionally performed, but often avoided to prevent tumor spread; definitive diagnosis typically follows surgical removal.
Physical Examination: Evaluates signs of hormonal excess.
Imaging Tests: CT scans, MRIs, or PET scans to visualize tumor size and spread.
Blood and Urine Tests: Identify abnormal hormone levels.
Stages
Types of Treatment
Overview of Treatment Modalities
Treatment depends on tumor type, stage, and patient’s health:
- Surgery:
- Adrenalectomy: Removal of the affected adrenal gland, the mainstay for localized tumors.
- Debulking Surgery: Reduces tumor burden in advanced cases.
- Radiation Therapy:
- Targets residual cancer cells post-surgery or addresses inoperable tumors.
- Chemotherapy:
- Mitotane: A key agent used to suppress hormone production and destroy cancer cells.
- Other drugs (e.g., cisplatin, etoposide) for advanced disease.
- Targeted Therapy:
- Focuses on specific genetic mutations in adrenal cancer cells.
- Clinical Trials:
- Investigational treatments and drug combinations for advanced or resistant ACC.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Surgery | Removes tumor | Pain, infection | >50% for localized cases | Smith et al., 2021 |
| Radiation | Shrinks/eliminates residual cells | Fatigue, skin irritation | Effective for residual disease | Lee et al., 2020 |
| Chemotherapy | Targets rapidly dividing cells | Nausea, fatigue | Moderate for advanced cases | Carter et al., 2023 |
| Targeted Tx | Blocks specific genetic pathways | Diarrhea, fatigue | Promising in trials | Brown et al., 2022 |
Living with Cancer
Living with adrenal cancer requires a holistic approach:
- Hormonal Management: Medications to balance hormone levels during/after treatment.
- Nutritional Support: Balanced diet to maintain energy and stable weight.
- Emotional Support: Counseling or support groups to cope with diagnosis and treatment.
- Regular Monitoring: Follow-up imaging and hormone testing to detect recurrence.
Additional Resources
Key Takeaways
- Adrenal cancer is aggressive, demanding swift diagnosis and intervention.
- Symptoms often involve hormonal imbalances or abdominal discomfort.
- Treatment may include surgery, radiation, chemotherapy, and emerging targeted therapies.
- Ongoing follow-up is crucial for managing recurrences and maintaining quality of life.
Final Recommendations
- Recognize symptoms such as hormonal imbalances or unexplained weight changes, and seek timely evaluation.
- Discuss all treatment options—including clinical trials—with your healthcare provider.
- Adopt supportive care measures (e.g., nutritional guidance, psychological support) to improve overall well-being.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Adrenal Cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
