Book Appointment Now
Understanding Blood Cancer

Blood Cancer Guide
Introduction
Blood cancers, also known as hematologic malignancies, are a diverse group of cancers that affect the blood, bone marrow, and lymphatic system. The main types include leukemia, lymphoma, and multiple myeloma. Historically, these cancers were considered fatal due to limited understanding and lack of effective treatments. However, significant advancements over the past few decades have transformed the prognosis for many patients. The introduction of targeted therapies, immunotherapies, and stem cell transplantation has improved survival rates and quality of life. Studying blood cancers is crucial because they account for a substantial portion of cancer-related morbidity and mortality worldwide, and ongoing research continues to uncover novel therapeutic strategies.
Statistics
Global Incidence and Mortality
According to the Global Cancer Observatory (GLOBOCAN) 2022 data:
- Leukemia:
- Incidence: Approximately 487,000 new cases worldwide.
- Mortality: Around 305,000 deaths globally.
- Lymphoma:
- Non-Hodgkin Lymphoma (NHL):
- Incidence: Approximately 553,389 new cases.
- Mortality: About 250,679 deaths.
- Hodgkin Lymphoma:
- Incidence: Around 82,469 new cases.
- Mortality: Approximately 22,733 deaths.
- Non-Hodgkin Lymphoma (NHL):
- Multiple Myeloma:
- Incidence: Approximately 187,952 new cases.
- Mortality: Around 121,388 deaths.
Key Disparities
- Gender:
- Age:
- Leukemia:
- Acute Lymphoblastic Leukemia (ALL): Most common in children.
- Acute Myeloid Leukemia (AML): Incidence increases with age.
- Lymphoma:
- Hodgkin Lymphoma: Peaks in young adults (15-35 years) and those over 55.
- NHL: Risk increases with age.
- Multiple Myeloma: Primarily affects individuals over 65 years.
- Leukemia:
- Geography:
- Higher Incidence Regions:
- Leukemia: North America, Europe, Australia.
- Lymphoma: Higher NHL rates in North America and Europe.
- Multiple Myeloma: More common in developed countries.
- Lower Incidence Regions:
- Africa and Asia generally have lower reported rates, but may be underrepresented due to limited diagnostic capabilities.
- Higher Incidence Regions:
Key Statistics
- Leukemia:
- 5-Year Survival Rates:
- ALL in Children: Over 90% in high-income countries.
- AML in Adults: Around 30%.
- Chronic Myeloid Leukemia (CML): Exceeds 80% with tyrosine kinase inhibitor (TKI) therapy.
- 5-Year Survival Rates:
- Lymphoma:
- Hodgkin Lymphoma:
- 5-Year Survival Rate: Over 85%.
- Non-Hodgkin Lymphoma:
- 5-Year Survival Rate: Varies from 60-85% depending on subtype and stage.
- Hodgkin Lymphoma:
- Multiple Myeloma:
- 5-Year Survival Rate: Approximately 55%, improved due to novel therapies.
Trends Over Time
- Increasing Survival Rates:
- Advancements in treatment have significantly improved survival for many blood cancers.
- Example: Introduction of TKIs in CML increased 10-year survival from 20% to over 80%.
- Stable or Slightly Increasing Incidence Rates:
- Some blood cancers show stable incidence, while others, like NHL, have seen slight increases, possibly due to better detection and aging populations.
Source: International gco.iarc.who.int
Medical Illustrations
Comparing Healthy & Cancerous Blood Cells:
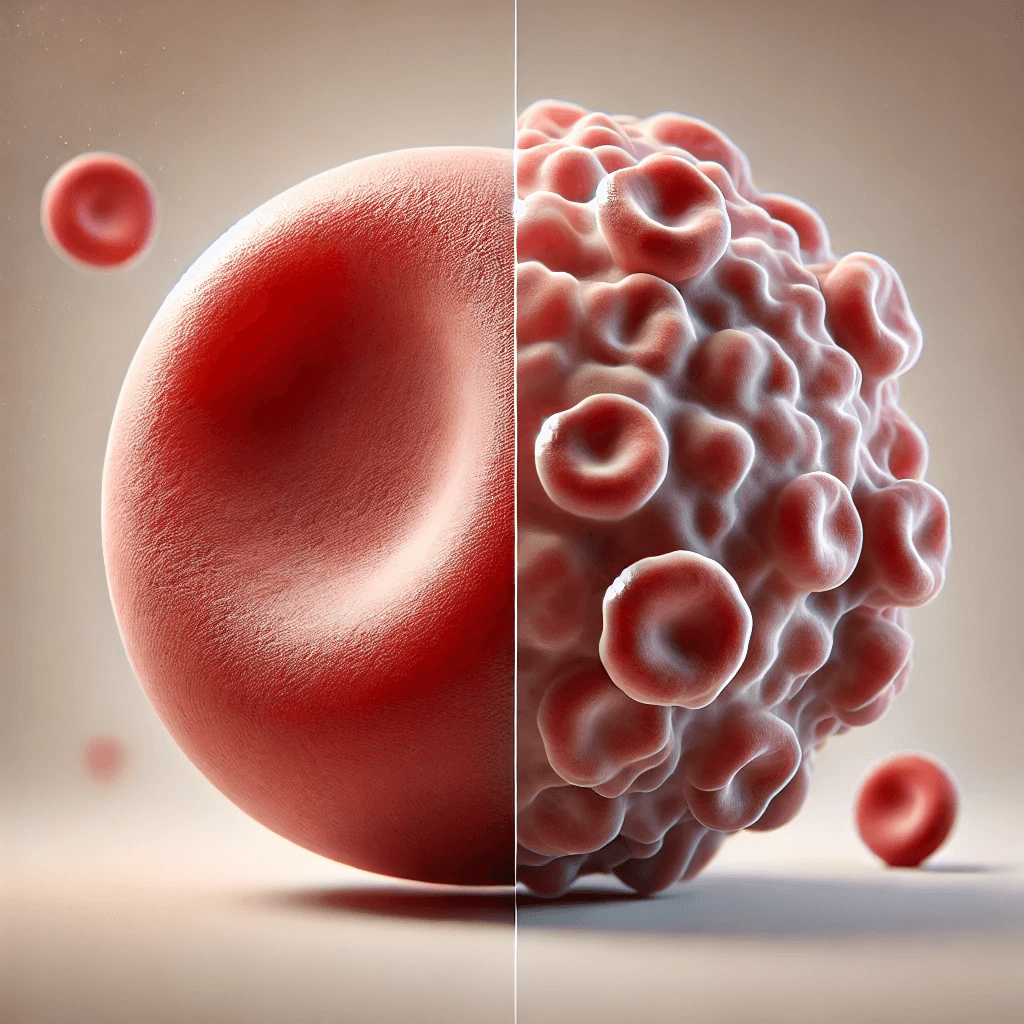
Blood cancer cells:

Risk Factors and Prevention
a. Known Risk Factors
Environmental Exposures:
- Radiation:
- High-dose exposure (e.g., atomic bomb survivors) increases leukemia risk.
- Therapeutic radiation in previous cancers may elevate risk.
- Chemicals:
- Benzene Exposure:
- Found in industrial settings.
- Linked to AML and other leukemias.
- Benzene Exposure:
- Chemotherapy:
- Certain chemotherapeutic agents can be leukemogenic.
Genetic Predisposition:
- Inherited Syndromes:
- Down Syndrome:
- Increases risk of ALL and AML.
- Fanconi Anemia:
- Associated with AML.
- Li-Fraumeni Syndrome:
- Mutation in TP53 gene increases various cancer risks, including blood cancers.
- Down Syndrome:
- Family History:
- Slightly elevated risk if a first-degree relative has a hematologic malignancy.
Infections:
- Human T-cell Lymphotropic Virus Type 1 (HTLV-1):
- Associated with adult T-cell leukemia/lymphoma.
- Epstein-Barr Virus (EBV):
- Linked to Burkitt lymphoma and Hodgkin lymphoma.
Lifestyle Factors:
- Smoking:
- Increases risk of AML.
- Obesity:
- Associated with higher incidence of multiple myeloma.
Recent Studies:
- A meta-analysis in Blood (2021) confirmed benzene exposure significantly increases leukemia risk.
- Research in Leukemia (2022) identified obesity as a modifiable risk factor for multiple myeloma.
b. Preventive Strategies
Lifestyle Modifications:
- Smoking Cessation:
- Reduces risk of AML over time.
- Weight Management:
- Healthy diet and exercise may lower multiple myeloma risk.
Occupational Safety:
- Exposure Reduction:
- Implementing safety measures to minimize benzene exposure in industrial settings.
- Regulations:
- Enforcing limits on workplace exposure to known carcinogens.
Infection Control:
- Screening Blood Products:
- Reduces transmission of HTLV-1 and other oncogenic viruses.
- Antiviral Therapies:
- Managing chronic viral infections may reduce associated cancer risks.
Avoiding Unnecessary Radiation and Chemotherapy:
- Medical Practices:
- Limiting exposure to diagnostic radiation when possible.
- Using chemotherapeutic agents judiciously.
Genetic Counseling:
- For individuals with family histories of inherited syndromes, counseling can inform risk and guide monitoring.
Vaccination:
- Hepatitis B and C Vaccination:
- Indirectly reduces risk of certain lymphomas associated with chronic infections.
Note: Currently, there are no specific vaccines or chemopreventive agents approved for preventing blood cancers.
Screening
Current Screening Methods
Lack of Routine Screening:
- Rationale:
- Blood cancers are relatively rare and often present with nonspecific symptoms.
- No cost-effective, widely accepted screening tests for asymptomatic individuals.
High-Risk Population Monitoring:
- Genetic Syndromes:
- Individuals with conditions like Down syndrome may undergo regular blood counts and clinical evaluations.
- Occupational Exposures:
- Workers exposed to benzene may receive periodic health screenings.
Early Detection Strategies:
- Awareness of Symptoms:
- Educating the public and healthcare providers to recognize early signs.
- Research Efforts:
- Investigating biomarkers and genetic tests that could enable future screening.
Comparative Summary:
- No Standard Screening for the general population due to lack of effective methods.
- Targeted Monitoring in high-risk groups may aid early detection.
Symptoms and Signs
Early-Stage Symptoms:
- General Symptoms:
- Fatigue and weakness.
- Fever or night sweats.
- Unexplained weight loss.
Intermediate-Stage Symptoms:
- Anemia:
- Shortness of breath.
- Pallor.
- Leukopenia:
- Frequent infections.
- Thrombocytopenia:
- Easy bruising or bleeding gums.
- Swollen Lymph Nodes:
- Especially in lymphoma.
- Bone Pain:
- Common in multiple myeloma.
Late-Stage Symptoms:
- Organomegaly:
- Enlarged spleen or liver.
- Neurological Symptoms:
- Headaches, visual disturbances (especially in ALL).
- Hypercalcemia:
- Nausea, constipation, confusion (in multiple myeloma).
Misdiagnoses and Atypical Presentations:
- Case Anecdote:
- A 45-year-old man treated repeatedly for recurrent infections later diagnosed with chronic lymphocytic leukemia (CLL) after routine blood work revealed lymphocytosis.
- Challenges:
- Symptoms are often nonspecific and can mimic common illnesses.
- Delay in diagnosis may occur due to subtle initial findings.
Diagnosis Steps
- Initial Evaluation:
- Medical History:
- Assess symptoms, exposure risks, family history.
- Physical Examination:
- Check for lymphadenopathy, hepatosplenomegaly, signs of anemia or bleeding.
- Medical History:
- Laboratory Tests:
- Complete Blood Count (CBC):
- Evaluate for anemia, leukopenia/leukocytosis, thrombocytopenia.
- Peripheral Blood Smear:
- Assess morphology of blood cells.
- Blood Chemistry:
- Renal and liver function tests, calcium levels (important in multiple myeloma).
- Complete Blood Count (CBC):
- Bone Marrow Examination:
- Bone Marrow Aspiration and Biopsy:
- Gold standard for diagnosing leukemia and multiple myeloma.
- Determines cellular morphology and percentage of blasts.
- Bone Marrow Aspiration and Biopsy:
- Immunophenotyping:
- Flow Cytometry:
- Identifies cell surface markers to classify leukemia or lymphoma subtype.
- Flow Cytometry:
- Cytogenetic and Molecular Analyses:
- Karyotyping:
- Detects chromosomal abnormalities (e.g., Philadelphia chromosome in CML).
- Polymerase Chain Reaction (PCR):
- Identifies specific gene rearrangements or mutations.
- Next-Generation Sequencing (NGS):
- Comprehensive genetic profiling.
- Karyotyping:
- Imaging Studies:
- X-rays:
- Detect bone lesions in multiple myeloma.
- CT Scan and PET-CT:
- Assess lymph node involvement and staging in lymphoma.
- MRI:
- Evaluate CNS involvement.
- X-rays:
- Additional Tests:
- Lumbar Puncture:
- Checks for CNS involvement in ALL.
- Urine Protein Electrophoresis:
- Detects Bence Jones proteins in multiple myeloma.
- Lumbar Puncture:
- Staging and Risk Stratification:
- Leukemia:
- Classified based on cell type and genetic abnormalities.
- Lymphoma:
- Ann Arbor staging system.
- Multiple Myeloma:
- International Staging System (ISS) based on beta-2 microglobulin and albumin levels.
- Leukemia:
Stages
Types of Treatment
Treatment Modalities
Chemotherapy:
- Mechanism:
- Kills rapidly dividing cells by interfering with DNA replication.
- Indications:
- Mainstay for acute leukemias and aggressive lymphomas.
- Outcomes:
- Induces remission in many cases.
- Side Effects:
- Hair loss, nausea, myelosuppression, risk of infections.
Radiation Therapy:
- Mechanism:
- Uses high-energy radiation to destroy cancer cells.
- Indications:
- Hodgkin lymphoma, localized NHL, CNS involvement.
- Outcomes:
- Effective for localized disease.
- Side Effects:
- Fatigue, skin reactions, long-term risk of secondary cancers.
Targeted Therapy:
- Tyrosine Kinase Inhibitors (TKIs):
- Agents: Imatinib, dasatinib, nilotinib.
- Mechanism: Inhibit BCR-ABL tyrosine kinase in CML.
- Side Effects: Edema, muscle cramps, cytopenias.
- Efficacy: Long-term remission in CML patients.
- Monoclonal Antibodies:
- Agents: Rituximab (targets CD20), daratumumab (targets CD38).
- Mechanism: Bind to specific antigens on cancer cells, inducing cell death.
- Side Effects: Infusion reactions, immunosuppression.
- Efficacy: Improved survival in lymphomas and multiple myeloma.
Immunotherapy:
- Chimeric Antigen Receptor (CAR) T-cell Therapy:
- Mechanism: Patient’s T-cells are modified to attack cancer cells.
- Indications: Refractory B-cell ALL, certain NHLs.
- Outcomes: High remission rates in refractory cases.
- Side Effects: Cytokine release syndrome, neurotoxicity.
- Immune Checkpoint Inhibitors:
- Agents: Nivolumab, pembrolizumab.
- Mechanism: Block inhibitory pathways to enhance immune response.
- Side Effects: Autoimmune reactions.
- Efficacy: Effective in certain Hodgkin lymphoma cases.
Stem Cell Transplantation:
- Autologous Transplant:
- Mechanism: Patient’s own stem cells are collected, high-dose chemotherapy administered, then stem cells reinfused.
- Indications: Multiple myeloma, relapsed lymphoma.
- Outcomes: Prolongs remission.
- Side Effects: Risk of infections, graft failure.
- Allogeneic Transplant:
- Mechanism: Stem cells from a donor are transplanted.
- Indications: High-risk leukemias, relapsed diseases.
- Outcomes: Potential for cure through graft-versus-leukemia effect.
- Side Effects: Graft-versus-host disease (GVHD), infections.
Supportive Care:
- Blood Transfusions:
- Treat anemia and thrombocytopenia.
- Growth Factors:
- Stimulate white blood cell production.
- Antibiotics and Antifungals:
- Prevent or treat infections.
Evidence-Based Comparisons
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Imatinib | TKI inhibiting BCR-ABL tyrosine kinase | Edema, muscle cramps, cytopenias | 10-year OS >80% in CML patients | IRIS Trial, 2003 |
| CAR T-cell Therapy | Modified T-cells targeting CD19 antigen | Cytokine release syndrome, neurotoxicity | ORR ~82% in refractory large B-cell lymphoma | ZUMA-1 Trial, 2017 |
| Rituximab + Chemotherapy | Anti-CD20 antibody plus chemo | Infusion reactions, immunosuppression | 5-year OS >70% in NHL patients | Coiffier et al., 2002 |
| Daratumumab | Anti-CD38 antibody | Infusion reactions, cytopenias | Improved PFS in relapsed multiple myeloma | CASTOR Trial, 2016 |
Key Studies:
- IRIS Trial (2003):
- Findings: Imatinib showed superior survival in CML compared to interferon-alpha plus cytarabine.
- Clinical Significance: Established imatinib as first-line therapy for CML.
- ZUMA-1 Trial (2017):
- Findings: CAR T-cell therapy achieved an overall response rate of 82% in refractory large B-cell lymphoma.
- Clinical Significance: Led to FDA approval of axi-cel for certain NHL patients.
Additional Resources
- Patient Advocacy Groups:
- Key Opinion Leaders:
- Dr. Brian Druker: Pioneer in developing TKIs for CML.
- Dr. Carl June: Leader in CAR T-cell therapy research.
- Clinical Trials:
- ClinicalTrials.gov: Database of ongoing blood cancer studies.
- National Cancer Institute Trials
Key Findings
- Advancements in Treatment: Targeted therapies and immunotherapies have significantly improved survival rates in blood cancers.
- Importance of Personalized Medicine: Genetic and molecular profiling guides effective treatment strategies.
- Limited Prevention and Screening: No standard screening methods; emphasis on awareness and early symptom recognition.
- Risk Factors Identified: Environmental exposures and genetic predispositions play roles in development.
- Challenges Remain: Access to advanced treatments varies globally; resistance mechanisms need further research.
Discussion
The introduction of targeted therapies and immunotherapies has revolutionized the management of blood cancers. For instance, TKIs like imatinib have transformed CML from a fatal disease into a manageable chronic condition for many patients. Similarly, monoclonal antibodies and CAR T-cell therapies have significantly improved outcomes in lymphomas and multiple myeloma.
Personalized medicine, guided by genetic and molecular profiling, allows for tailored treatments that enhance efficacy and reduce unnecessary toxicity. The identification of specific mutations and biomarkers facilitates the selection of appropriate therapies and prognostic assessments.
Despite these advancements, challenges persist. There is a lack of effective screening methods for early detection in the general population, making awareness of symptoms critical. Disparities in access to advanced diagnostics and treatments contribute to variable outcomes across different regions and socioeconomic groups.
Resistance to therapies remains a significant hurdle. Understanding the mechanisms behind resistance can lead to the development of new strategies to overcome it and improve long-term survival.
Final Recommendations
Clinical Recommendations:
- Emphasize Personalized Medicine:
- Utilize genetic and molecular profiling to guide treatment decisions.
- Enhance Access to Advanced Therapies:
- Work towards making novel treatments available globally.
- Monitor for Resistance:
- Regularly assess treatment effectiveness and adjust strategies as needed.
Research Directions:
- Investigate Resistance Mechanisms:
- Focus on understanding how cancers evade current therapies.
- Develop Early Detection Methods:
- Research biomarkers that could enable screening in high-risk populations.
- Explore New Therapeutic Targets:
- Identify novel molecular pathways for drug development.
Public Health Policy Suggestions:
- Increase Awareness:
- Implement educational campaigns about blood cancer symptoms and risk factors.
- Promote Occupational Safety:
- Enforce regulations to reduce exposure to known carcinogens.
- Support Funding for Research:
- Allocate resources towards blood cancer research and treatment accessibility.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including blood cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
