Book Appointment Now
Understanding Lung Cancer
Lung Cancer Guide
Introduction
Lung cancer is one of the most prevalent and deadly forms of cancer worldwide. Historically associated primarily with tobacco smoking, lung cancer has been a focal point of oncology research for decades. In recent years, significant advancements have been made in understanding its molecular biology, leading to the development of targeted therapies and immunotherapies that have improved patient outcomes. Studying lung cancer is critically important due to its high incidence and mortality rates, the emergence of cases in non-smokers, and the potential for early detection to significantly improve survival rates.
Statistics
Statistical Overview
Globally, lung cancer remains the leading cause of cancer-related deaths. According to the World Health Organization (WHO), in 2020:
- Incidence: Approximately 2.2 million new cases were diagnosed worldwide.
- Mortality: Around 1.8 million deaths were attributed to lung cancer.
Key Disparities
- Gender:
- Men: Historically higher incidence and mortality rates, though rates are decreasing due to reduced smoking.
- Women: Incidence rates are stabilizing or increasing in some regions, reflecting past smoking trends.
- Age:
- Most cases occur in individuals over 65 years.
- Rising incidence in younger, non-smoking populations highlights the need for further research.
- Geography:
- High-Income Countries: Incidence rates are stabilizing or declining due to effective tobacco control measures.
- Low- and Middle-Income Countries: Increasing incidence due to rising tobacco use and exposure to environmental carcinogens.
Key Statistics
- 5-Year Survival Rates:
- Overall: Approximately 20%.
- Localized Disease: Up to 60%, emphasizing the importance of early detection.
- Regional Spread: Around 33%.
- Distant Metastasis: Less than 6%.
- Trends Over Time:
- Decreasing Mortality in Men: Reflecting declines in smoking prevalence.
- Stable or Increasing Mortality in Women: Due to historical smoking patterns and possibly other risk factors.
Global Lung Cancer Incidence and Mortality Rates
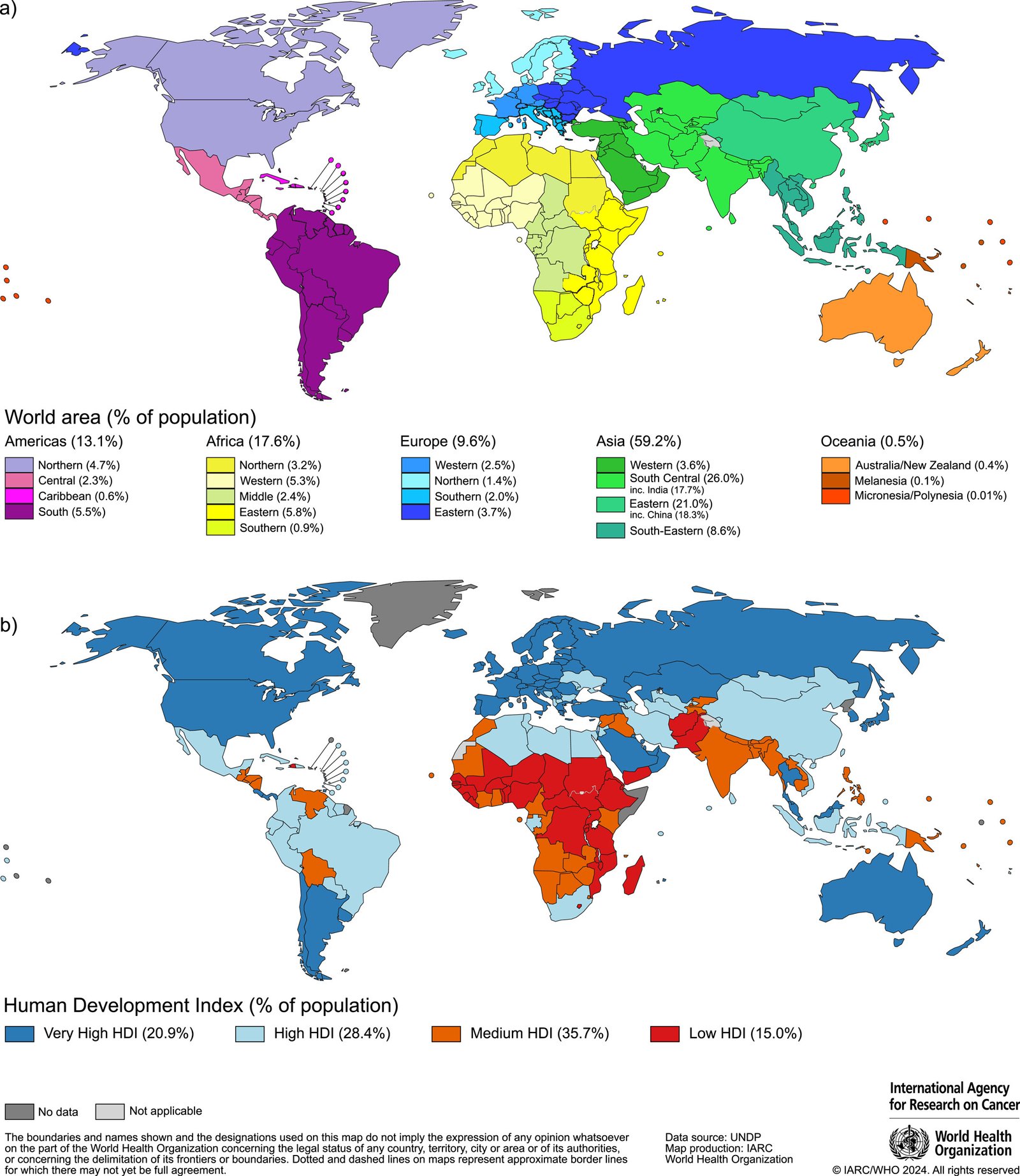
Source: International Agency for Research on Cancer (IARC)
Medical Illustrations
- Lung cancer:

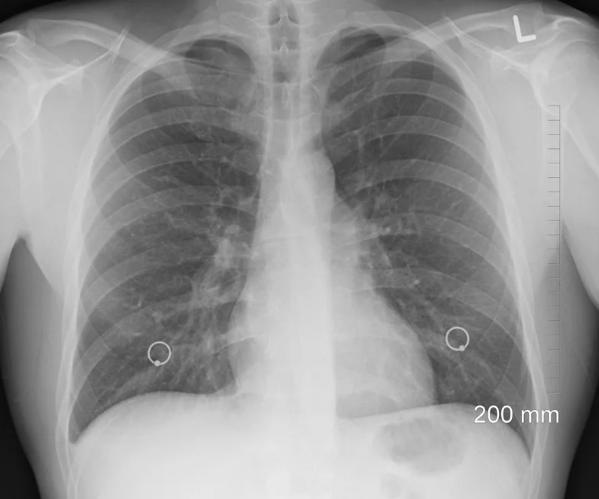
CT Lung tumor:
Risk Factors and Prevention
Known Risk Factors
Environmental Factors:
- Tobacco Smoking:
- Active Smoking: The leading cause, responsible for approximately 85% of lung cancer cases.
- Secondhand Smoke: Increases risk by 20–30% in non-smokers.
- Occupational Exposures:
- Asbestos: Strongly linked to mesothelioma and lung cancer.
- Radon Gas: Second leading cause in the U.S.; radioactive gas found in homes.
- Silica and Diesel Exhaust: Associated with increased risk.
- Air Pollution:
- Particulate Matter (PM2.5): Long-term exposure linked to higher incidence.
Genetic Factors:
- Family History: First-degree relatives with lung cancer may double one’s risk.
- Genetic Mutations:
- EGFR, ALK, KRAS mutations can predispose individuals, particularly non-smokers.
Other Factors:
- Radiation Therapy: Previous radiation to the chest increases risk.
- Chronic Lung Diseases: Conditions like COPD and pulmonary fibrosis are associated with higher risk.
Recent Studies:
Research in Nature Genetics (2021) identified novel genetic variants associated with lung cancer susceptibility in non-smokers.
A meta-analysis in The Lancet Oncology (2022) highlighted the synergistic effect of smoking and occupational exposures on lung cancer risk.
Preventive Strategies
Lifestyle Changes:
- Smoking Cessation:
- Effectiveness: Quitting reduces risk over time; after 15 years, the risk approaches that of non-smokers.
- Support Programs: Behavioral therapy, nicotine replacement, and medications improve cessation success rates.
- Avoiding Secondhand Smoke: Policies banning indoor smoking protect non-smokers.
Environmental Measures:
- Radon Mitigation: Testing and reducing radon levels in homes.
- Occupational Safety: Regulations to limit exposure to carcinogens like asbestos and silica.
Chemoprevention:
- Beta-Carotene Supplements:
- Evidence: Large trials like the ATBC study found increased lung cancer risk in smokers taking beta-carotene supplements.
- Recommendation: Avoid high-dose supplements in smokers.
Vaccination Strategies:
- Currently, no vaccines prevent lung cancer directly, but research into therapeutic vaccines is ongoing.
Screening
Current Screening Methods
Low-Dose Computed Tomography (LDCT):
- Efficacy:
- Mortality Reduction: The National Lung Screening Trial (NLST) showed a 20% reduction in lung cancer mortality with LDCT screening in high-risk individuals.
- Sensitivity and Specificity:
- Sensitivity: Approximately 93.8%, meaning it detects most cases.
- Specificity: Around 73.4%, leading to some false positives.
- Risks and Benefits:
- Benefits: Early detection allows for surgical intervention, improving survival rates.
- Risks: False positives can lead to unnecessary procedures; exposure to low radiation doses.
- Cost Effectiveness:
- Considered cost-effective for high-risk populations due to reduced mortality.
- Practicality:
- Recommended for adults aged 55–80 with a 30 pack-year smoking history, who currently smoke or have quit within the past 15 years.
Chest X-Ray and Sputum Cytology:
- Efficacy:
- Less sensitive than LDCT; not recommended for screening.
- Risks and Benefits:
- Minimal risks but lower detection rates.
Emerging Screening Methods:
- Biomarker Tests:
- Research into blood-based biomarkers (e.g., circulating tumor DNA) is ongoing.
- Potential: Non-invasive and could complement LDCT in the future.
Comparative Summary:
- LDCT is the only recommended screening modality for high-risk individuals due to its proven mortality benefit.
- Chest X-Ray and Sputum Cytology are not effective for screening purposes.
Symptoms and Signs
Early-Stage Symptoms:
- Often asymptomatic; underscores the importance of screening in high-risk populations.
Intermediate-Stage Symptoms:
- Persistent Cough: One of the most common early symptoms.
- Hemoptysis: Coughing up blood.
- Shortness of Breath: Due to airway obstruction.
- Chest Pain: May worsen with deep breathing or coughing.
Advanced-Stage Symptoms:
- Unintentional Weight Loss: Significant weight loss without trying.
- Fatigue: Generalized weakness and lack of energy.
- Hoarseness: If the tumor affects the laryngeal nerve.
- Bone Pain: Indicates possible metastasis.
- Neurological Symptoms: Headaches, seizures, or dizziness if spread to the brain.
Misdiagnoses and Atypical Presentations:
- Case Anecdote: A 45-year-old non-smoker presenting with shoulder pain was initially treated for musculoskeletal issues before imaging revealed a Pancoast tumor.
- Challenges: Symptoms can mimic other conditions like pneumonia or chronic bronchitis, leading to delays in diagnosis.
Diagnosis Steps
- Initial Evaluation:
- Medical History: Evaluate symptoms and family history.
- Physical Examination: Check for abdominal masses or tenderness.
- Imaging Studies:
- Chest X-Ray: Initial assessment to detect masses.
- Low-Dose CT Scan: Provides detailed images of lung lesions.
- PET-CT Scan: Evaluates metabolic activity and helps in staging.
- Laboratory Tests:
- Complete Blood Count (CBC): Checks for anemia or elevated white blood cells.
- Blood Chemistry Tests: Assesses organ function.
- Biopsy Procedures:
- Bronchoscopy with Biopsy: Visualizes airways and collects tissue samples.
- CT-Guided Needle Biopsy: Used for peripheral lung lesions.
- Thoracoscopy or Thoracotomy: Surgical options for obtaining tissue.
- Pathological Analysis:
- Histological Examination: Determines cancer type (NSCLC vs. SCLC).
- Molecular Testing: Identifies genetic mutations (EGFR, ALK, ROS1).
- Staging:
- TNM Classification: Assesses tumor size (T), lymph node involvement (N), and metastasis (M).
- Additional Tests:
- Carcinoembryonic Antigen (CEA): Baseline level for monitoring treatment response.
Stages
Types of Treatment
Treatment Modalities
Surgery:
- Indications: Early-stage NSCLC without metastasis.
- Procedures:
- Lobectomy: Removal of a lung lobe; standard surgical approach.
- Pneumonectomy: Removal of an entire lung; reserved for extensive tumors.
- Segmentectomy or Wedge Resection: For small, localized tumors.
- Side Effects: Risk of infection, bleeding, reduced lung function.
Radiation Therapy:
- Usage: Used alone or in combination; also for palliation in advanced stages.
- Types:
- External Beam Radiation Therapy (EBRT).
- Stereotactic Body Radiotherapy (SBRT): High-dose radiation to small areas.
- Side Effects: Fatigue, skin reactions, esophagitis.
Chemotherapy:
- Common Regimens: Platinum-based therapies like cisplatin or carboplatin combined with other agents.
- Mechanism: Kills rapidly dividing cells by damaging DNA.
- Side Effects: Nausea, vomiting, hair loss, increased infection risk.
Immunotherapy:
- Agents:
- PD-1 Inhibitors: Nivolumab, Pembrolizumab.
- PD-L1 Inhibitors: Atezolizumab.
- Mechanism: Enhances the immune system’s ability to recognize and destroy cancer cells.
- Side Effects: Immune-related adverse events like colitis, pneumonitis.
Targeted Therapies:
- Agents:
- EGFR Inhibitors: Osimertinib, Erlotinib.
- ALK Inhibitors: Alectinib, Crizotinib.
- Mechanism: Blocks specific molecules involved in tumor growth.
- Side Effects: Diarrhea, rashes, liver function abnormalities.
Evidence-Based Comparisons
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Chemotherapy | Damages DNA of rapidly dividing cells | Nausea, hair loss, fatigue | Median OS ~10–12 months in advanced NSCLC | Scagliotti et al., 2008 |
| Immunotherapy | Blocks PD-1/PD-L1 pathway to boost immunity | Fatigue, rash, pneumonitis | Median OS ~16–18 months in advanced NSCLC | KEYNOTE-189, 2018 |
| Targeted Therapy (EGFR Inhibitors) | Inhibits EGFR tyrosine kinase | Diarrhea, rash, stomatitis | Median PFS ~18.9 months in EGFR-mutated NSCLC | FLAURA Trial, 2018 |
| Combination Therapy (Chemo + Immuno) | Combines cytotoxic and immune effects | Combined side effects | Improved OS and PFS compared to chemo alone | KEYNOTE-189, 2018 |
Key Studies:
- KEYNOTE-189 (2018):
- Findings: Pembrolizumab plus chemotherapy significantly improved overall survival compared to chemotherapy alone.
- Clinical Significance: Established combination therapy as first-line treatment for metastatic non-squamous NSCLC without EGFR or ALK mutations.
- FLAURA Trial (2018):
- Findings: Osimertinib improved progression-free survival compared to first-generation EGFR inhibitors.
- Clinical Significance: Recommended as first-line therapy for EGFR-mutated NSCLC.
Additional Resources
- Patient Advocacy Groups:
- Key Opinion Leaders:
- Dr. Alice Shaw: Expert in ALK-positive lung cancer.
- Dr. Roy Herbst: Leader in immunotherapy research.
- Clinical Trials:
- ClinicalTrials.gov: Database for ongoing lung cancer studies.
- National Cancer Institute Trials
- Advocacy organization
Key Findings
- Lung Cancer Remains the Leading Cause of Cancer Death: High mortality underscores the need for continued research and prevention efforts.
- Smoking is the Primary Risk Factor: Smoking interruption significantly reduces risk.
- Advancements in Personalized Medicine: Targeted therapies and immunotherapies have improved outcomes for specific patient groups.
- Early Detection Improves Survival: LDCT screening reduces mortality in high-risk populations.
- Emerging Risk in Non-Smokers: Increasing cases highlight the need to investigate other risk factors.
Discussion
The decline in lung cancer incidence and mortality among men in high-income countries reflects successful tobacco control measures. However, the increasing rates among women and in low- to middle-income countries are concerning. The high mortality rate is partly due to late-stage diagnosis; thus, implementing effective screening programs is crucial.
Advancements in molecular biology have revolutionized treatment, allowing for targeted therapies that improve survival and quality of life. Immunotherapies have opened new avenues for treatment, though challenges like resistance and identifying suitable candidates remain.
Discrepancies in access to care and advanced treatments contribute to survival differences globally. Additionally, the rise in lung cancer among non-smokers necessitates research into environmental and genetic factors, including air pollution and radon exposure.
Final Recommendations
Clinical Recommendations:
- Promote Smoking Cessation: Integrate interruption programs into primary care and oncology settings.
- Implement LDCT Screening: Recommend for high-risk individuals to facilitate early detection.
- Utilize Molecular Testing: Perform genetic profiling for all advanced NSCLC cases to guide targeted therapy.
Research Directions:
- Investigate Non-Smoker Lung Cancer: Focus on environmental exposures and genetic predispositions.
- Develop Biomarkers: Identify reliable predictors for treatment response and resistance.
- Explore Combination Therapies: Study synergistic effects of immunotherapies with other treatments.
Policy Suggestions:
- Strengthen Tobacco Control: Enforce regulations on advertising, increase taxes, and promote public education.
- Improve Access to Care: Ensure availability of screening and advanced treatments in underserved areas.
- Environmental Regulations: Reduce air pollution and occupational exposures through stricter policies.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including lung cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
