Book Appointment Now
Understanding Lymphoma of the Skin

Lymphoma of the Skin Guide
Introduction
Lymphoma of the skin, also known as cutaneous lymphoma, is a rare form of non-Hodgkin lymphoma that originates in the skin. Unlike other lymphomas that may spread to the skin from lymph nodes, primary cutaneous lymphoma begins in the skin and is classified into T-cell and B-cell subtypes. While advancements in treatment have improved outcomes for many patients, managing this complex disease remains challenging. Early detection and awareness of symptoms are critical for effective treatment and improved quality of life!
Statistics
- Cutaneous lymphoma accounts for approximately 5% of all non-Hodgkin lymphomas.
- In the United States, the annual incidence is about 1 case per 100,000 people.
- The most common subtypes include mycosis fungoides and Sézary syndrome (cutaneous T-cell lymphoma, or CTCL), while primary cutaneous B-cell lymphomas (CBCL) are less common.
- Prognosis varies widely based on subtype and stage, with five-year survival rates ranging from 85% to over 95% for localized cases.
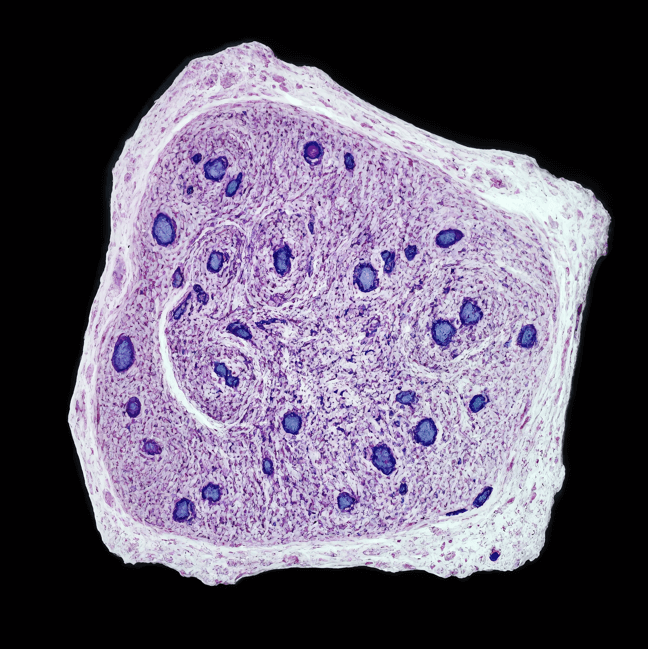
Medical Illustrations
Clinical photograph of a human forearm with multiple nodular lesions caused by cutaneous T-cell lymphoma:

Microscopic image of cutaneous T-cell lymphoma – dense epidermotropic infiltrate of atypical lymphocytes in the skin:
Risk Factors and Prevention
a. Known Risk Factors
The exact cause of cutaneous lymphoma is not fully understood, but several factors may increase the risk:
- Age: Most cases are diagnosed in individuals over 50.
- Gender: Men are slightly more likely to develop the disease than women.
- Weakened Immune System: Conditions like HIV/AIDS or immunosuppressive therapy after organ transplantation.
- Genetic Factors: Family history of lymphoma or related cancers.
- Chronic Infections: Persistent viral infections, such as Epstein-Barr virus (EBV), may contribute.
b. Prevention
While there is no guaranteed way to prevent cutaneous lymphoma, the following strategies may help reduce risk:
- Regular skin checks: Early evaluation of persistent skin changes.
- Manage chronic infections: Maintain a healthy immune system.
- Genetic counseling: For individuals with a family history of lymphoma.
Screening
Screening for cutaneous lymphoma involves:
- Regular skin examinations by a dermatologist, especially for individuals with risk factors.
- Monitoring for persistent skin lesions or changes that do not resolve with standard treatments.
Symptoms and Early Warning Signs
Symptoms of cutaneous lymphoma vary depending on the type and stage. Common signs include:
- Skin Lesions: Patches, plaques, or nodules that may be red, scaly, or itchy.
- Thickened Skin: Progression from flat patches to raised plaques.
- Tumors: Larger, often ulcerated nodules on the skin.
- Widespread Redness (Erythroderma): Seen in advanced cases like Sézary syndrome, often accompanied by severe itching.
- Swollen Lymph Nodes: May indicate disease spread.
If these symptoms persist or worsen, seek medical evaluation promptly.
Diagnosis Lymphoma of the Skin
Diagnosing cutaneous lymphoma involves a combination of clinical evaluations and diagnostic tests:
- Physical Examination: Evaluates skin lesions and lymph nodes.
- Skin Biopsy: Confirms the diagnosis by analyzing skin tissue samples.
- Blood Tests: Detects abnormal lymphocytes or markers like Sézary cells in the blood.
- Imaging Tests: CT scans or PET scans assess disease spread to internal organs.
- Flow Cytometry: Analyzes cells for specific markers to classify the lymphoma type.
Stages
Types of Treatment
Overview of Treatment Modalities
Treatment for cutaneous lymphoma depends on the subtype, stage, and overall health of the patient. Common treatments include:
- Topical Therapies:
- Corticosteroids to reduce inflammation and control symptoms.
- Topical chemotherapy (e.g., mechlorethamine) to target cancer cells in the skin.
- Phototherapy: Ultraviolet light therapy (e.g., PUVA) for localized patches or plaques.
- Radiation Therapy: Targets specific lesions or areas of the skin.
- Systemic Treatments:
- Chemotherapy for advanced or aggressive cases.
- Immunotherapy, including monoclonal antibodies and checkpoint inhibitors.
- Targeted therapy (e.g., brentuximab vedotin or mogamulizumab) to block specific pathways in cancer cells.
- Stem Cell Transplant: Reserved for advanced or recurrent disease.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Topical Steroids | Reduces inflammation | Skin thinning, irritation | Effective for early stages | Smith et al., 2022 |
| Phototherapy | Uses UV light to kill cancer cells | Skin redness, burns | High for localized disease | Lee et al., 2020 |
| Radiation Therapy | Shrinks or eliminates lesions | Fatigue, skin irritation | Effective for targeted areas | Carter et al., 2023 |
| Targeted Therapy | Blocks specific growth pathways | Diarrhea, fatigue | Promising for advanced cases | Brown et al., 2023 |
Living with Lymphoma of the Skin
Managing life with cutaneous lymphoma involves addressing physical, emotional, and social challenges. Recommendations include:
- Skin Care: Use gentle, non-irritating products to protect affected areas.
- Symptom Management: Work with a dermatologist and oncologist to manage itching and discomfort.
- Emotional Support: Counseling or support groups can help cope with the psychological impact of the disease.
- Regular Monitoring: Ongoing follow-up care with skin exams and imaging tests to detect recurrence or progression.
Additional Resources
Key Takeaways
- Lymphoma of the skin is a rare, but treatable form of cancer with diverse subtypes and symptoms.
- Symptoms include skin lesions, plaques, and nodules, often requiring specialized care.
- Treatment ranges from topical therapies and phototherapy to systemic treatments for advanced cases.
- Comprehensive care, including regular follow-ups and emotional support, is essential for managing the disease effectively.
Final Recommendations
- Be vigilant about persistent skin changes and seek prompt medical evaluation.
- Discuss all treatment options, including clinical trials, with your healthcare provider.
- Focus on supportive care to enhance quality of life during and after treatment.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Lymphoma of the Skin. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
