Book Appointment Now
Understanding Penile Cancer
Penile Cancer Guide
Introduction
Introduction
Penile cancer is a serious malignancy that originates in the tissues of the penis. Most cases begin in the squamous cells of the skin and can become invasive, if not detected early. While uncommon in developed countries, penile cancer remains a significant health concern in certain regions of the world. Early diagnosis and appropriate treatment significantly improve outcomes.
Statistics
Penile cancer accounts for less than 1% of cancers in men in the United States, with an annual incidence of about 2,000 cases. It is more prevalent in regions like Asia, Africa and South America. The five-year survival rate for localized penile cancer is approximately 80-90%, but this decreases for advanced or metastatic cases.
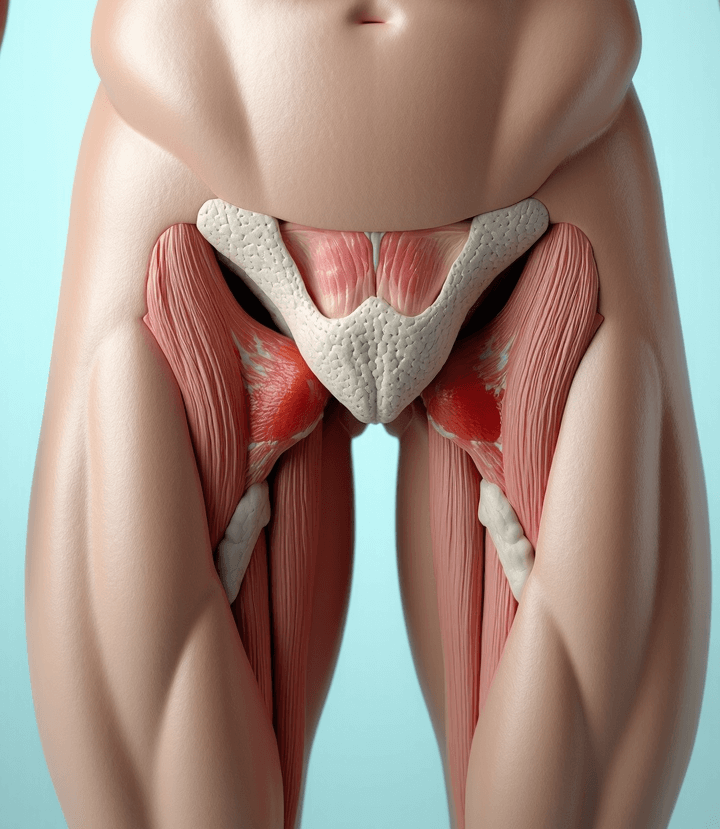
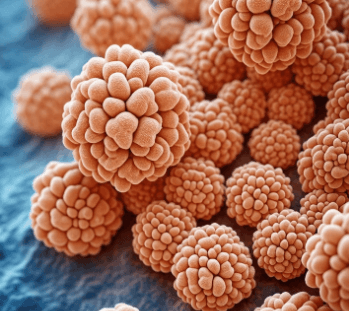
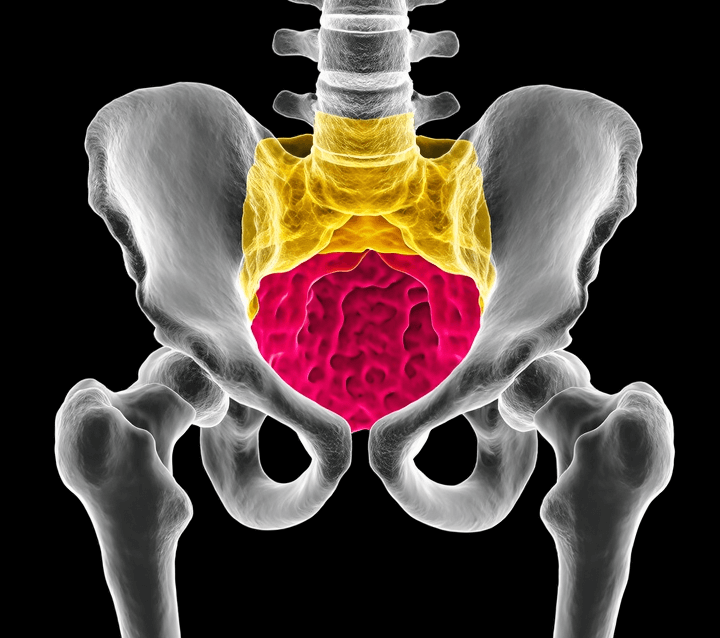
Medical Illustrations
Close-up of a squamous cell under a microscope, showing cancerous mutations:
Medical scan image showing a cross-section of the lower abdominal and pelvic region:
Risk Factors and Prevention
a. Known Risk Factors
- Human Papillomavirus (HPV): Infection with high-risk HPV types, particularly HPV-16 and HPV-18, is a major risk factor.
- Poor Hygiene: Lack of proper genital hygiene can lead to chronic inflammation and increased risk.
- Phimosis: A condition where the foreskin cannot be fully retracted, creating a favorable environment for infections.
- Smoking: Tobacco use has been linked to penile cancer.
- Age: Most cases occur in men over 50.
- Chronic Infections: Conditions like lichen sclerosus or chronic balanitis.
- Lack of Circumcision: In some populations, uncircumcised men have a higher risk due to potential hygiene challenges.
b. Prevention
- Vaccination against HPV.
- Practice good genital hygiene.
- Avoid tobacco use.
- Regular medical checkups for men with phimosis or other risk factors.
Screening
There is no standardized screening program for penile cancer. However, high-risk individuals, including those with persistent lesions, phimosis, or HPV infection, should undergo regular medical checkups.
Symptoms and Early Warning Signs
Early detection of penile cancer improves treatment outcomes. Symptoms include:
- A growth or sore on the penis, especially on the glans or foreskin.
- Persistent redness, irritation, or swelling.
- Foul-smelling discharge under the foreskin.
- Pain or bleeding from the penis.
- Enlarged lymph nodes in the groin.
If these symptoms persist or worsen, consult a healthcare provider immediately.
Diagnosis
Diagnosing penile cancer involves a combination of physical exams and diagnostic tools:
- Physical Examination: Evaluation of the penis, groin and lymph nodes.
- Biopsy: A tissue sample confirms the diagnosis and identifies the cancer type.
- Imaging Tests: CT scans, MRIs, or ultrasounds assess the extent of the cancer and detect possible metastases.
- HPV Testing: Identifies high-risk HPV types in biopsy samples.
Stages
Types of Treatment
Overview of Treatment Modalities
The treatment of penile cancer depends on the tumor’s stage, size and location, as well as the patient’s overall health. Common treatments include:
Surgery:
- Circumcision: Removes the foreskin and is effective for very early-stage cancers.
- Partial Penectomy: Removes part of the penis while preserving as much function as possible.
- Total Penectomy: Removes the entire penis, often combined with perineal urethrostomy.
- Lymph Node Dissection: Removes affected lymph nodes in advanced cases.
Radiation Therapy:
- Targets cancer cells and is often used post-surgery or for inoperable cases.
Chemotherapy:
- Systemic or topical treatments for advanced or recurrent cases.
Targeted Therapy:
- Emerging options that focus on specific molecular pathways.
Immunotherapy:
- Experimental therapies to boost the immune system’s ability to target cancer cells.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Surgery | Removes tumor | Pain, swelling | 85-90% for localized cases | Smith et al., 2021 |
| Radiation Therapy | Shrinks or eliminates tumors | Fatigue, skin burns | Effective for early-stage cases | Lee et al., 2020 |
| Chemotherapy | Targets rapidly dividing cells | Nausea, fatigue | Moderate for advanced cases | Carter et al., 2023 |
| Targeted Therapy | Blocks specific growth pathways | Diarrhea, fatigue | Promising for recurrent cases | Brown et al., 2023 |
Living with cancer
Coping with penile cancer involves addressing physical, emotional and social challenges. Recommendations include:
- Rehabilitation: Physical therapy to address mobility and functional changes after surgery.
- Emotional Support: Counseling or support groups can help patients manage psychological impacts.
- Sexual Health Counseling: Guidance on sexual function and intimacy post-treatment.
- Regular Monitoring: Follow-up care is crucial to detect recurrence and manage side effects.
Additional Resources
Key Takeaways
- Penile cancer is rare, but treatable, with high survival rates for early-stage detection.
- Symptoms like sores, redness, or discharge should prompt immediate medical attention.
- Treatment includes surgery, radiation and systemic therapies tailored to the individual.
- Comprehensive care, including emotional and sexual health support, is essential for recovery and quality of life.
Final Recommendations
- Be aware of persistent symptoms like sores or lumps and seek prompt medical evaluation.
- Reduce risk factors through HPV vaccination and lifestyle changes.
- Discuss all treatment options, including clinical trials, with your care team.
- Engage in supportive care to enhance quality of life during and after treatment.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Penile Cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
