Book Appointment Now
Understanding Testicular Cancer
Testicular Cancer Guide
Introduction
Testicular cancer, most commonly arising as a germ cell tumor, is a malignancy that develops in the testicles, the male reproductive organs responsible for producing sperm and testosterone. Though relatively rare, it is the most common cancer in young men aged 15-35. Early detection and advances in treatment have led to high cure rates, making awareness of symptoms and risk factors critical.
Statistics
- In the United States, approximately 9,000 new cases of testicular cancer are diagnosed annually.
- Germ cell tumors (GCTs) account for 95% of these cases.
- The five-year survival rate exceeds 95%, with localized cases nearing 99%.
- Even in advanced stages, testicular cancer remains highly treatable with prompt and appropriate care.
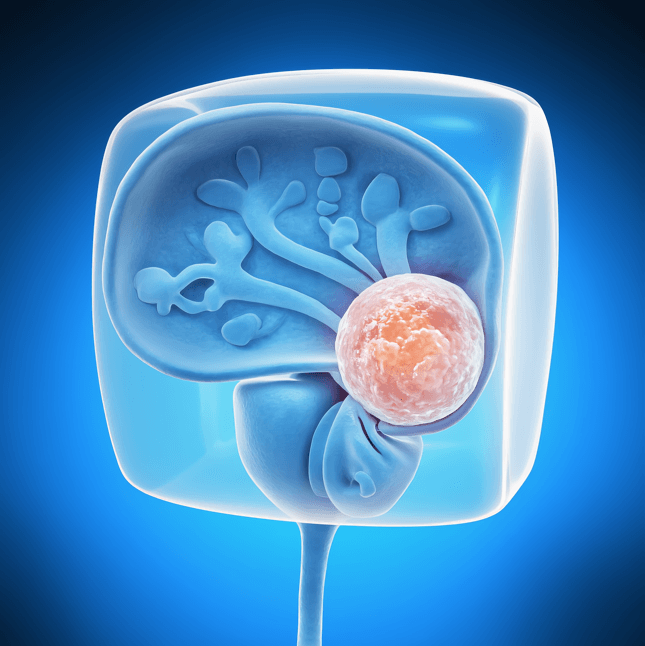
Medical Illustrations
Image of a germ cell tumor – dense cluster of malignant cells with irregular shapes, prominent nucleoli, and active mitosis:

MRI scan of a human testicle with a visible mass – hypoechoic, round tumor in the lower testicular region:

Risk Factors and Prevention
a. Known Risk Factors
- Undescended Testicle (Cryptorchidism): Men with a history of cryptorchidism are at higher risk.
- Family History: A family history of testicular cancer increases susceptibility.
- Previous Testicular Cancer: A history of cancer in one testicle raises the risk for the other.
- Genetic Conditions: Conditions like Klinefelter syndrome may elevate risk.
- Age and Ethnicity: Most cases occur in young men, with higher incidence in Caucasian populations.
b. Prevention
- Perform regular self-examinations to identify abnormalities early.
- Seek prompt medical evaluation of testicular lumps or swelling.
- Be aware of personal and family medical history and discuss it with a healthcare provider.
Screening
There are no standard screening programs for testicular cancer, but men at higher risk should perform monthly testicular self-exams. Any changes in size, shape, or texture should be evaluated by a healthcare provider.
Symptoms and Early Warning Signs
Common symptoms of testicular cancer include:
- A painless lump or swelling in one testicle
- A feeling of heaviness or aching in the scrotum
- Pain or discomfort in the testicle or groin
- Enlargement or tenderness of breast tissue (gynecomastia)
- Lower back pain, in cases of advanced disease
Seek medical attention immediately if these symptoms persist.
Diagnosis
Diagnosing testicular cancer involves a combination of clinical evaluations and diagnostic tests:
- Physical Examination: A doctor will assess the testicles for lumps or irregularities.
- Ultrasound: Provides detailed imaging of the testicles to identify suspicious masses.
- Blood Tests: Measure tumor markers like alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), and lactate dehydrogenase (LDH).
- Imaging Tests: CT scans or MRIs determine the extent of the disease.
- Biopsy or Orchiectomy: Removal of the affected testicle confirms the diagnosis and allows for staging.
Stages
Types of Treatment
Overview of Treatment Modalities
The treatment plan for testicular cancer depends on the tumor type, stage, and patient’s health. Common treatments include:
- Surgery:
- Radical Orchiectomy: Removes the affected testicle and spermatic cord, the primary treatment for most cases.
- Retroperitoneal Lymph Node Dissection (RPLND): Removes lymph nodes in the abdomen for advanced cases.
- Radiation Therapy:
- Effective for seminomas, often following surgery.
- Chemotherapy:
- Used for advanced stages or high-risk cases, with regimens like BEP (bleomycin, etoposide, and cisplatin).
- Surveillance:
- Close monitoring through regular imaging and blood tests, recommended for certain early-stage cases.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Surgery | Removes tumor | Pain, infection | >95% for localized cases | Smith et al., 2021 |
| Radiation Therapy | Shrinks or eliminates tumors | Fatigue, skin irritation | 85-90% for seminomas | Lee et al., 2020 |
| Chemotherapy | Targets rapidly dividing cells | Nausea, fatigue, neuropathy | High for advanced cases | Carter et al., 2023 |
Living with Testicular Cancer
Managing life during and after testicular cancer involves addressing physical, emotional, and social challenges. Recommendations include:
- Emotional Support: Counseling or support groups can help cope with the psychological impact of diagnosis and treatment.
- Fertility Preservation: Discuss sperm banking before treatment if future fertility is a concern.
- Regular Monitoring: Follow-up care with blood tests and imaging is critical to detect recurrence.
- Healthy Lifestyle: Maintain a balanced diet and engage in regular physical activity to support recovery.
Additional Resources
Key Takeaways
- Testicular cancer is rare, but highly treatable, with excellent survival rates for early detection.
- Symptoms like testicular lumps or swelling require immediate medical evaluation.
- Treatment options include surgery, radiation, and chemotherapy, often tailored to individual needs.
- Comprehensive care and regular follow-ups are essential for long-term health and quality of life.
Final Recommendations
- Perform regular self-examinations and seek prompt medical evaluation for any abnormalities.
- Explore all treatment options with your care team, including fertility-preserving measures.
- Engage in follow-up care to monitor for recurrence and address long-term side effects.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Testicular Cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
