Book Appointment Now
Understanding Basal Cell Carcinoma

Basal Cell Carcinoma Guide
Introduction
What Is Basal Cell Carcinoma?
Basal cell carcinoma (BCC) is the most common type of skin cancer. It begins in the basal cells, which are located in the deepest layer of the epidermis (the outer layer of the skin). BCC usually develops on areas of the skin that are frequently exposed to the sun, such as the face, neck, and hands.
Why Is It Important to Learn About Basal Cell Carcinoma?
Understanding BCC is crucial because:
- High Prevalence: BCC is the most occurring form of all cancers.
- Early Detection Leads to Successful Treatment: When detected early, BCC is highly treatable and rarely life-threatening.
- Prevention Is Possible: Many cases can be prevented through sun protection and awareness.
Recent Developments:
- Improved Treatments: Advances in surgical techniques and topical medications have enhanced treatment outcomes.
- Awareness Campaigns: Increased public education on sun safety has helped in early detection and prevention.
Statistical Overview
Incidence:
- BCC accounts for about 8 out of 10 skin cancers diagnosed in the United States.
- Approximately 3.6 million cases of BCC are diagnosed in the U.S. each year.
Mortality Rate:
- BCC is rarely fatal. Death from BCC is extremely uncommon.
Survival Rate:
- The survival rate is very high when BCC is detected and treated early.
Trends and Disparities:
- Age Factors:
- BCC most commonly occurs in older adults, typically those over 50 years old.
- The incidence is increasing in younger adults due to sun exposure behaviors.
Gender Differences:
- Historically more common in men, but rates in women are rising.
Geographic Variations:
- Higher incidence in regions with intense sunlight, such as Australia and southern parts of the United States.
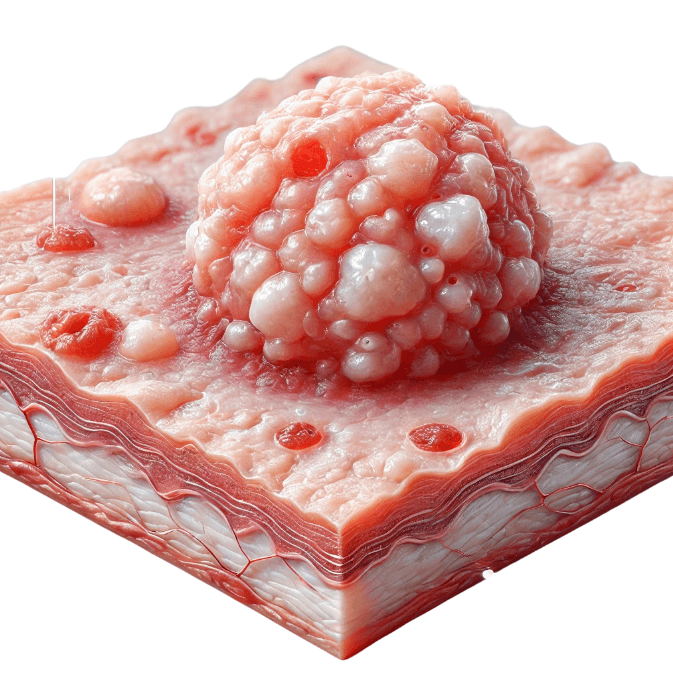
Medical Illustrations
Different types of basal cell carcinoma:
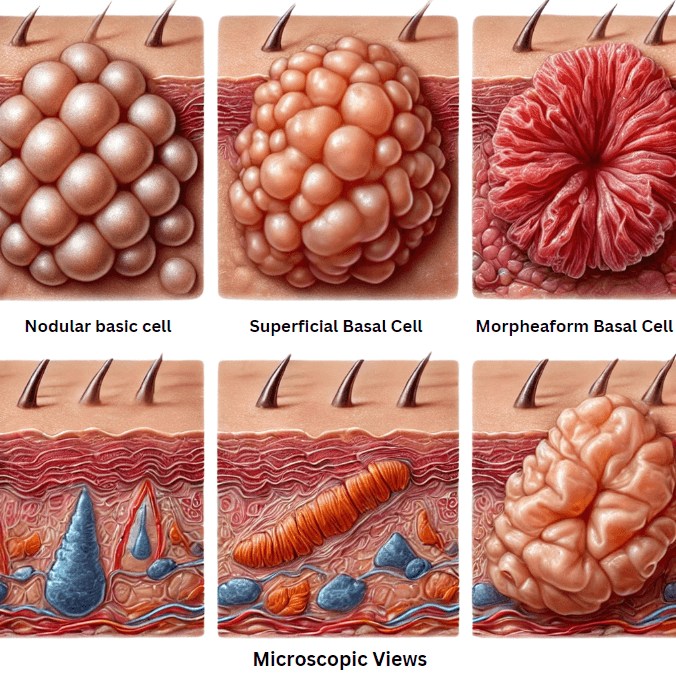
Medical illustration of basal cell carcinoma:
Risk Factors and Prevention
a. Known Risk Factors
- Excessive Sun Exposure:
- Ultraviolet (UV) Radiation: Frequent exposure to UV radiation from the sun or tanning beds increases risk.
- Fair Skin:
- People with light skin, blond or red hair, blue or green eyes, and freckles have less melanin, offering less natural protection.
- Age:
- Risk increases as you get older due to cumulative sun exposure.
- Personal or Family History:
- Previous skin cancer increases the likelihood of developing BCC again.
- Radiation Therapy:
- Past radiation treatments can raise the risk in the treated area.
- Chronic Skin Conditions:
- Conditions causing long-term skin inflammation or injury.
- Immune System Suppression:
- People with weakened immune systems, such as organ transplant recipients, are at higher risk.
- Exposure to Certain Substances:
- Contact with arsenic (a toxic metal) can increase risk.
b. Prevention
Protect Your Skin from UV Radiation:
- Use Sunscreen:
- Apply broad-spectrum sunscreen with at least SPF 30 daily.
- Reapply every two hours and after swimming or sweating.
- Wear Protective Clothing:
- Long-sleeved shirts, pants, wide-brimmed hats, and UV-blocking sunglasses.
- Seek Shade:
- Especially between 10 a.m. and 4 p.m., when the sun’s rays are strongest.
- Avoid Tanning Beds:
- They emit harmful UV radiation that can damage skin cells.
Regular Skin Examinations:
- Self-Exams:
- Check your skin monthly for any new changes.
- Professional Skin Exams:
- Visit a dermatologist annually or as recommended.
Healthy Lifestyle Choices:
- Avoid Smoking:
- Smoking can impair skin health and healing.
- Balanced Diet and Hydration:
- Supports overall skin health.
Recent Studies Support:
- Sunscreen Efficacy:
- Regular sunscreen use can significantly reduce the risk of developing BCC (Journal of Clinical Oncology, 2011).
Screening
Screening Methods:
1. Self-Examination:
Regularly inspect your skin for any changes or new growths.
2. Professional Skin Examination:
Dermatologists can identify suspicious lesions through visual inspection.
Symptoms and Signs
Common Symptoms:
- New Growths or Sores:
- A pearly white or waxy bump on the skin, often with visible blood vessels.
- A flat, scaly, reddish patch with a raised edge.
- Open Sores:
- Sores that bleed, ooze, or crust and do not heal over a few weeks.
- Scar-Like Area:
- A white, yellow, or waxy area with poorly defined borders; the skin appears shiny or tight.
- Persistent Redness or Irritation:
- In some cases, BCC may appear as a persistent, non-healing area of skin.
Note: BCC commonly occurs on sun-exposed areas like the face, ears, neck, scalp, shoulders, and back.
When to Seek Medical Attention:
- If you notice any new, changing, or unusual skin growths.
- Sores that do not heal within four weeks.
Possible Confusions:
- BCC can be mistaken for non-cancerous skin conditions like eczema or psoriasis.
- Always consult a healthcare provider for proper evaluation.
Diagnosis
Diagnostic Process:
- Initial Evaluation:
- Physical Exam: Doctor examines the skin lesion.
- Dermatoscopy:
- A dermatoscope magnifies the skin to provide a clearer view of the lesion.
- Skin Biopsy:
- Procedure:
- A small sample of the skin lesion is removed under local anesthesia.
- Types of Biopsies:
- Punch Biopsy: Uses a circular tool to remove a small core of skin.
- Excisional Biopsy: Entire lesion is removed.
- Purpose:
- The sample is examined under a microscope to confirm diagnosis.
- Procedure:
Understanding Results:
- Positive for BCC:
- The presence of cancerous basal cells.
- Further Assessment:
- BCC rarely spreads, so additional tests are uncommon unless advanced disease is suspected.
Benefits of Early Diagnosis:
- Increases the likelihood of complete removal and cure.
- Minimizes scarring and the extent of surgery needed.
Stages
Types of Treatment
Overview of Treatment Modalities
- Surgical Treatments:
- Excisional Surgery:
- How It Works:
- The cancerous lesion and a margin of healthy skin are removed.
- Outcomes:
- High cure rates; standard treatment for most BCCs.
- Side Effects:
- Scarring, risk of infection (low).
- How It Works:
- Mohs Micrographic Surgery:
- How It Works:
- Layers of skin are removed and examined immediately until no cancer cells remain.
- Outcomes:
- Highest cure rates; preserves as much healthy tissue as possible.
- Side Effects:
- Minimal scarring; local anesthesia used.
- How It Works:
- Excisional Surgery:
- Non-Surgical Treatments:
- Topical Medications:
- Imiquimod Cream:
- Mechanism:
- Stimulates the immune system to attack cancer cells.
- Side Effects:
- Redness, swelling, itching at the application site.
- Mechanism:
- 5-Fluorouracil (5-FU) Cream:
- Mechanism:
- Chemotherapy drug applied to the skin to destroy cancer cells.
- Side Effects:
- Skin irritation, photosensitivity.
- Mechanism:
- Imiquimod Cream:
- Photodynamic Therapy (PDT):
- How It Works:
- A light-sensitive drug is applied to the skin and activated by a special light to destroy cancer cells.
- Side Effects:
- Redness, swelling, sensitivity to light.
- How It Works:
- Topical Medications:
- Radiation Therapy:
- How It Works:
- Uses high-energy rays to destroy cancer cells.
- When Used:
- For patients who cannot undergo surgery.
- Side Effects:
- Skin irritation, redness, long-term risk of skin changes.
- How It Works:
- Targeted Therapy:
- Hedgehog Pathway Inhibitors:
- Drugs:
- Vismodegib (Erivedge), Sonidegib (Odomzo).
- How It Works:
- Blocks molecular signals that promote cancer cell growth.
- When Used:
- For advanced BCC that cannot be treated with surgery or radiation.
- Side Effects:
- Muscle spasms, hair loss, taste changes, fatigue.
- Drugs:
- Hedgehog Pathway Inhibitors:
Comparing Treatments
| Treatment | How It Works | Common Side Effects | Effectiveness | Study/Trial |
|---|---|---|---|---|
| Surgery | Physically removes cancer | Scarring, low infection risk | Cure rates over 95% for primary BCC | Chen et al., 2019 |
| Mohs Surgery | Removes cancer layer by layer | Minimal scarring | Cure rates up to 99% for primary BCC | Nguyen et al., 2018 |
| Topical Therapy | Destroys cancer cells with medication | Skin irritation, redness | Effective for superficial BCC; cure rates 80-90% | Williams et al., 2020 |
| Radiation Therapy | Kills cancer cells with radiation | Skin changes, fatigue | Cure rates around 90% for small BCCs | Silva et al., 2017 |
| Targeted Therapy | Blocks growth signals in cancer cells | Muscle cramps, hair loss | Controls advanced BCC in 50-60% of cases | Sekulic et al., 2012 |
Living with Cancer
Managing Physical Health:
- Nutrition:
- Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
- Exercise:
- Engage in regular physical activity as recommended by your healthcare provider.
- Skin Care:
- Follow wound care instructions after treatment to promote healing.
- Sun Protection:
- Continue to protect your skin from UV exposure to prevent new cancers.
Emotional Support:
- Mental Health:
- It’s normal to experience a range of emotions after a cancer diagnosis.
- Seek support from mental health professionals if needed.
- Support Groups:
- Connect with others through local or online support groups.
- Communication:
- Talk openly with friends and family about your feelings and needs.
Practical Tips:
- Keep Medical Records:
- Maintain a file of your diagnosis, treatment plans, and follow-up care.
- Stay Informed:
- Learn about your condition to make informed decisions.
- Follow-Up Care:
- Attend all scheduled appointments to monitor for recurrence or new skin cancers.
Additional Resources
These organizations offer valuable information, support networks, and updates on the latest research and treatments.
Key Takeaways
- Basal Cell Carcinoma Is the Most Common Skin Cancer:
- Arises from the basal cells in the skin’s epidermis.
- Risk Factors Include:
- Excessive sun exposure, fair skin, age, and weakened immune system.
- Symptoms to Watch For:
- New skin growths, non-healing sores, or changes in existing lesions.
- Early Detection Is Crucial:
- Regular skin exams can lead to early treatment and high cure rates.
- Effective Treatments Are Available:
- Surgery, topical medications, radiation therapy, and targeted therapies.
- Prevention Is Possible:
- Protecting your skin from UV radiation significantly reduces risk.
- Living with BCC:
- Focus on physical health, emotional support, and ongoing skin protection.
- Support Is Available:
- Reach out to healthcare providers and support organizations for assistance.
- Remember: Taking proactive steps in sun protection and skin monitoring can make a significant difference in preventing basal cell carcinoma and ensuring effective treatment if diagnosed.
Final Recommendations
- Practice Sun Safety:
- Use sunscreen daily, wear protective clothing, and avoid peak sun hours.
- Regular Skin Examinations:
- Perform monthly self-exams and schedule annual dermatologist visits.
- Avoid Tanning Beds:
- Steer clear of artificial UV sources.
- Protect Your Skin Year-Round:
- UV radiation can affect the skin even on cloudy days or during winter.
- Be Vigilant:
- Monitor your skin for any changes and report them to your healthcare provider promptly.
- Healthy Lifestyle Choices:
- Maintain a balanced diet, exercise regularly, and avoid smoking to support overall health.
- Educate Yourself and Others:
- Share information about BCC prevention and early detection with friends and family.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Basal Cell Carcinoma. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
