Book Appointment Now
Understanding Uterine Sarcoma

Uterine Sarcoma Guide
Introduction
Uterine sarcoma is a rare and aggressive form of cancer that originates in the muscles or connective tissues of the uterus. Unlike endometrial carcinoma, which develops in the lining of the uterus, uterine sarcomas arise in the structural or supporting tissues. Early detection can be challenging due to nonspecific symptoms, making awareness of risk factors and prompt diagnosis critical for effective treatment.
Statistics
Uterine sarcomas account for about 3-7% of all uterine cancers. In the United States, approximately 1,200 new cases are diagnosed annually. The most common subtypes include:
- Leiomyosarcoma (LMS): The most prevalent and aggressive subtype.
- Endometrial Stromal Sarcoma (ESS): A slower-growing, hormone-sensitive variant.
- Undifferentiated Uterine Sarcoma: A rare and highly aggressive form.
The five-year survival rate varies by subtype and stage, ranging from 50% for localized cases to less than 20% for advanced-stage disease.
Medical Illustrations
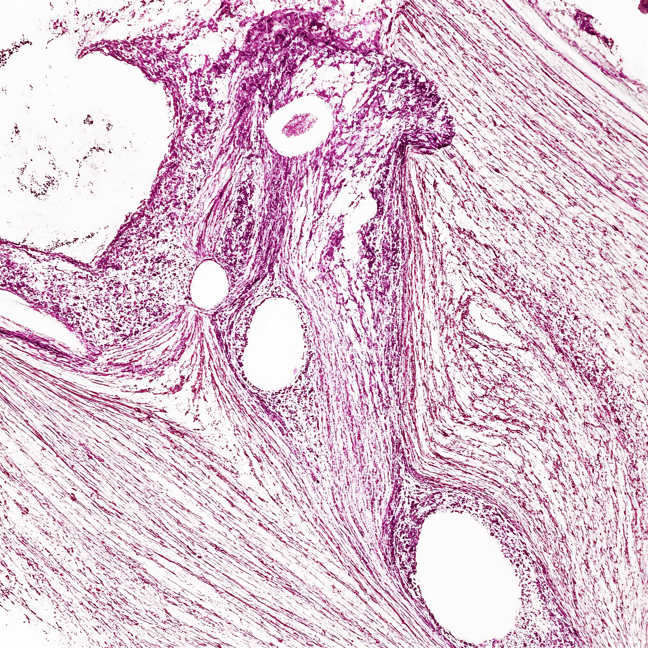
Microscopic image of uterine leiomyosarcoma – dense fascicles of spindle-shaped malignant cells with atypical nuclei, high mitotic activity, eosinophilic cytoplasm:
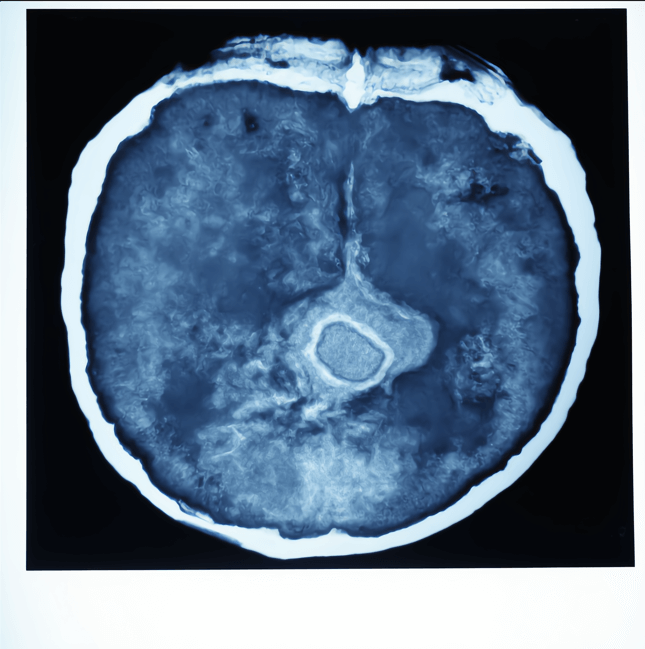
CT scan of a female pelvis showing a large irregular uterine mass suggestive of uterine sarcoma – heterogeneous density, with areas of necrosis and contrast enhancement:
Risk Factors and Prevention
a. Known Risk Factors
Several factors are associated with an increased risk of developing uterine sarcoma:
- Radiation Therapy: Previous pelvic radiation increases the likelihood of sarcoma development.
- Tamoxifen Use: Long-term use of tamoxifen for breast cancer treatment may elevate risk.
- Genetic Syndromes: Conditions such as hereditary leiomyomatosis and renal cell cancer (HLRCC) syndrome.
- Age: Most cases occur in postmenopausal women, typically over the age of 50.
- History of Uterine Fibroids: Though rare, fibroids may occasionally transform into sarcomas.
b. Prevention
- Routine gynecological checkups for early detection of uterine abnormalities.
- Discuss risks associated with tamoxifen use with your healthcare provider.
- Genetic counseling for individuals with a family history of HLRCC or similar syndromes.
Screening
There are no standard screening tests for uterine sarcoma. However, high-risk individuals (e.g., those with a history of pelvic radiation or genetic syndromes) should undergo regular pelvic exams and imaging when necessary.
Symptoms and Early Warning Signs
Symptoms of uterine sarcoma often overlap with other gynecological conditions, leading to delayed diagnosis. Common signs include:
- Abnormal uterine bleeding, especially postmenopausal bleeding
- Pelvic pain or pressure
- Unusual vaginal discharge, which may be foul-smelling
- A rapidly growing pelvic mass
- Frequent urination or difficulty emptying the bladder
If these symptoms persist, seek medical evaluation promptly.
Diagnosis Uterine Sarcoma
Diagnosing uterine sarcoma involves a combination of clinical evaluations and diagnostic tools:
- Pelvic Examination: Detects abnormalities in the uterus or surrounding tissues.
- Imaging Tests: Ultrasound, CT scans, or MRIs help visualize uterine masses and assess their characteristics.
- Endometrial Biopsy: Collects tissue samples from the uterine lining to rule out other conditions.
- Hysteroscopy: Provides a direct view of the uterine cavity for abnormalities.
- Surgical Biopsy or Dilation and Curettage (D&C): Confirms the diagnosis by analyzing tissue samples.
Stages
Types of Treatment
Overview of Treatment Modalities
The treatment of uterine sarcoma depends on the tumor’s type, stage, and the patient’s overall health. Common treatments include:
- Surgery:
- Hysterectomy: The primary treatment involves removing the uterus, and in some cases, the ovaries and fallopian tubes (bilateral salpingo-oophorectomy).
- Debulking Surgery: Removes as much of the tumor as possible in advanced cases.
- Radiation Therapy: Targets residual cancer cells and reduces recurrence risk.
- Chemotherapy: Administered for high-grade or advanced sarcomas, often using drugs like doxorubicin and ifosfamide.
- Hormonal Therapy: Used for certain low-grade tumors, particularly endometrial stromal sarcomas, with medications like progestins or aromatase inhibitors.
Comparing Treatments
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Surgery | Removes tumor | Pain, infection | 50-70% for localized cases | Smith et al., 2021 |
| Radiation Therapy | Shrinks or eliminates tumors | Fatigue, skin burns | Improves local control | Lee et al., 2020 |
| Chemotherapy | Targets rapidly dividing cells | Nausea, fatigue | Effective for advanced cases | Carter et al., 2023 |
| Hormonal Therapy | Blocks hormone receptors | Hot flashes, mood changes | Effective for hormone-sensitive tumors | Brown et al., 2022 |
Living with Cancer
Managing life with uterine sarcoma involves addressing physical, emotional, and practical challenges. Recommendations include:
- Rehabilitation: Physical therapy to improve mobility and strength after surgery.
- Pain Management: Work with specialists to alleviate chronic pain or treatment-related discomfort.
- Nutritional Support: Maintain a balanced diet to support recovery and overall health.
- Emotional Support: Seek counseling or join support groups for emotional well-being.
- Regular Monitoring: Follow-up care with imaging and blood tests to detect recurrence or manage side effects.
Additional Resources
Key Takeaways
- Uterine sarcoma is a rare, but aggressive cancer, requiring prompt diagnosis and treatment.
- Symptoms like abnormal bleeding and pelvic pain should not be ignored.
- Treatment includes surgery, radiation, chemotherapy, and hormonal therapy, tailored to the individual’s needs.
- Comprehensive care, including emotional and physical support, is essential for managing the disease and improving quality of life.
Final Recommendations
- Be proactive about recognizing symptoms like abnormal bleeding and seek timely medical evaluation.
- Discuss treatment options, including participation in clinical trials, with your healthcare provider.
- Focus on supportive care to improve quality of life during and after treatment.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including Uterine Sarcoma. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
