Book Appointment Now
Understanding Kidney Cancer
Kidney Cancer Guide
Introduction
Kidney cancer, also known as renal cancer, originates in the kidneys—two bean-shaped organs located on either side of the spine, responsible for filtering waste from the blood and producing urine. The most common type is renal cell carcinoma (RCC), accounting for approximately 90% of cases. Historically, kidney cancer was often diagnosed incidentally during imaging for unrelated issues due to its asymptomatic nature in early stages. Recent developments in molecular biology have led to targeted therapies and immunotherapies, significantly improving outcomes for advanced-stage patients. Studying kidney cancer is crucial due to its rising global incidence, the potential for early detection, and the advancements in personalized treatment approaches that can enhance patient survival and quality of life.
Statistics
Global Incidence and Mortality
According to the Global Cancer Observatory (GLOBOCAN) 2024 data:
- Incidence: Approximately 400,000 new cases of kidney cancer were diagnosed worldwide.
- Mortality: Around 175,000 deaths were attributed to kidney cancer globally.
Key Disparities
- Gender:
- Men: Higher incidence and mortality rates, with a male-to-female ratio of about 1.5:1.
- Women: Lower rates but still significantly affected.
- Age:
- Most commonly diagnosed between 60 and 70 years of age.
- Geography:
- Higher Incidence Regions:
- North America and Europe have higher incidence rates, possibly due to lifestyle factors and better diagnostic capabilities.
- Lower Incidence Regions:
- Asia and Africa report lower rates, but increasing trends are observed.
- Higher Incidence Regions:
Key Statistics
- 5-Year Survival Rates (based on the American Cancer Society data):
- Localized Disease (Stage I and II): Approximately 93%.
- Regional Spread (Stage III): Around 69%.
- Distant Metastasis (Stage IV): About 13%.
- Overall Survival Rate: Approximately 75%.
- Trends Over Time:
- Increasing Incidence: Partially due to improved imaging techniques leading to incidental findings.
- Stable or Slightly Decreasing Mortality Rates: Reflect advancements in treatment and early detection.
Global kidney cancer incidence and rates in 2022
| Country | Number | ASR/100,000 |
|---|---|---|
| World | 434,840 | 4.4 |
| China | 73,656 | 3.1 |
| United States of America | 71,759 | 12.8 |
| Russian Federation | 29,109 | 11.8 |
| Japan | 21,207 | 6.9 |
| Germany | 20,514 | 9.0 |
| India | 17,480 | 1.3 |
| France (metropolitan) | 14,541 | 11.4 |
| United Kingdom | 13,714 | 10.0 |
| Italy | 13,666 | 9.7 |
| Brazil | 11,090 | 3.9 |
Source: International wcrf.org
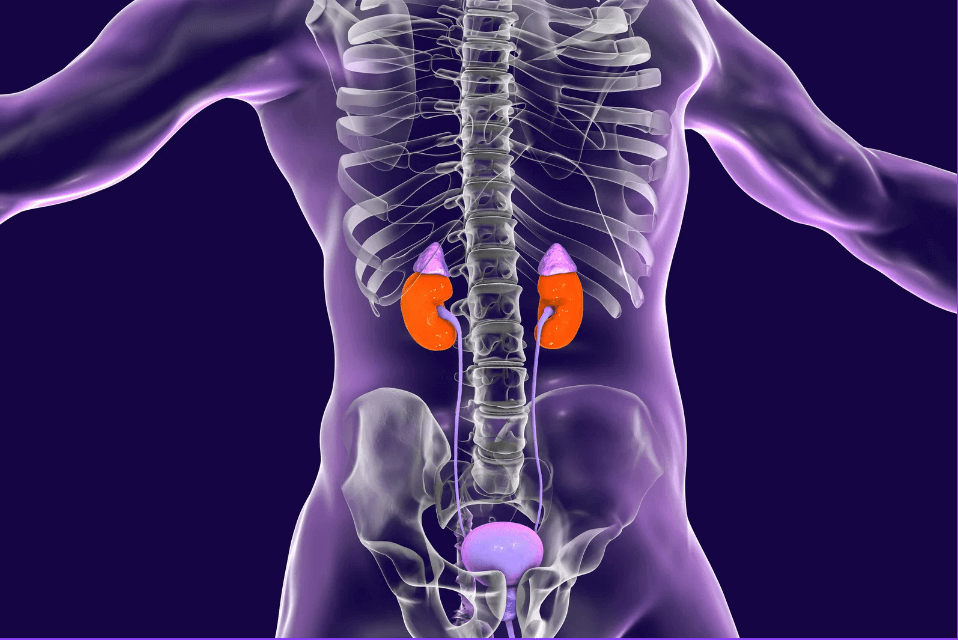
Medical Illustrations
Kidney system:

Large Kidney Tumour on CT Scan:

Risk Factors and Prevention
a. Known Risk Factors
Environmental and Lifestyle Factors:
- Smoking:
- Increases risk by approximately 50%.
- Mechanism: Carcinogens cause DNA damage in renal tubular cells.
- Obesity:
- Each 5 kg/m² increase in BMI is associated with a 24% higher risk.
- Mechanism: Hormonal imbalances, chronic inflammation.
- Hypertension:
- Long-standing high blood pressure is linked to increased risk.
- Mechanism: Renal damage leading to cellular changes.
- Occupational Exposures:
- Asbestos, cadmium, and trichloroethylene exposure increases risk.
Genetic Factors:
- Hereditary Syndromes:
- Von Hippel-Lindau (VHL) Disease:
- Mutations in the VHL gene; patients have a 35-45% lifetime risk.
- Hereditary Papillary RCC:
- MET proto-oncogene mutations.
- Birt-Hogg-Dubé Syndrome:
- FLCN gene mutations leading to chromophobe RCC.
- Von Hippel-Lindau (VHL) Disease:
Recent Studies:
- A meta-analysis in European Urology (2021) confirmed the association between obesity and increased RCC risk.
- Research in The New England Journal of Medicine (2020) identified new genetic mutations contributing to hereditary RCC.
b. Preventive Strategies
- Smoking Cessation:
- Reduces risk over time; former smokers have a lower risk than current smokers.
- Evidence: Cohort studies show decreased incidence after quitting.
- Weight Management:
- Healthy diet and regular exercise to maintain a normal BMI.
- Evidence: Studies suggest weight loss reduces risk factors.
- Blood Pressure Control:
- Managing hypertension through medication and lifestyle changes.
Occupational Safety:
- Exposure Reduction:
- Use of protective equipment to minimize contact with carcinogens.
- Regulatory Measures:
- Enforcement of safety standards in workplaces handling hazardous substances.
Chemoprevention:
- Currently, no medications are approved for RCC prevention.
Public Health Measures:
- Awareness Campaigns:
- Educate about modifiable risk factors.
- Screening in High-Risk Groups:
- Genetic counseling and surveillance for individuals with hereditary syndromes.
Screening
Current Screening Methods
Lack of Effective General Population Screening:
- Reasoning:
- Low incidence in the general population does not justify routine screening.
- No cost-effective, non-invasive tests with high sensitivity and specificity.
High-Risk Population Surveillance:
- Ultrasound and MRI:
- Usage:
- Recommended for individuals with hereditary syndromes.
- Efficacy:
- Sensitive in detecting early lesions.
- Risks and Benefits:
- Non-invasive with no radiation exposure (MRI).
- Costs may be prohibitive for routine use.
- Usage:
Incidental Findings:
- Imaging for Other Reasons:
- Many RCC cases are discovered incidentally during CT or MRI scans for unrelated issues.
- Impact:
- Leads to earlier detection and improved prognosis.
Comparative Summary:
- Routine Screening is not recommended for the general population.
- Targeted Surveillance in high-risk individuals can aid early detection.
Symptoms and Signs
Early-Stage Symptoms:
- Often asymptomatic; emphasizes the importance of incidental detection.
Intermediate-Stage Symptoms:
- Classic Triad (occurs in <10% of patients):
- Hematuria: Blood in urine.
- Flank Pain: Persistent pain on one side.
- Palpable Mass: Lump or mass in the abdomen or side.
- Other Symptoms:
- Unexplained weight loss.
- Fatigue.
- Fever not associated with infection.
Advanced-Stage Symptoms:
- Paraneoplastic Syndromes:
- Hypercalcemia: High calcium levels causing nausea, vomiting.
- Hypertension: Due to increased renin production.
- Metastatic Symptoms:
- Bone Pain: Indicates bone involvement.
- Cough or Shortness of Breath: If lungs are affected.
Misdiagnoses and Atypical Presentations:
- Case Anecdote:
- A 60-year-old patient treated for recurrent urinary tract infections later diagnosed with RCC after persistent hematuria.
- Challenges:
- Non-specific symptoms can delay diagnosis.
- Paraneoplastic syndromes may mislead clinicians.
Diagnosis Steps
- Initial Evaluation:
- Medical History:
- Evaluate risk factors: HBV/HCV status, alcohol use, family history.
- Physical Examination:
- Look for signs of chronic liver disease: jaundice, ascites, hepatomegaly.
- Medical History:
- Laboratory Tests:
- Urinalysis:
- Detects hematuria.
- Blood Tests:
- Complete blood count (CBC): Anemia or polycythemia.
- Serum electrolytes: Assess kidney function.
- Liver function tests: Rule out metastasis.
- Urinalysis:
- Imaging Studies:
- Ultrasound:
- Initial assessment to detect masses.
- Advantages: Non-invasive, no radiation.
- Computed Tomography (CT) Scan:
- Abdominal and Pelvic CT with Contrast:
- Gold standard for characterizing renal masses.
- Chest CT:
- Evaluates for pulmonary metastases.
- Abdominal and Pelvic CT with Contrast:
- Magnetic Resonance Imaging (MRI):
- Used when CT contrast is contraindicated.
- Superior for evaluating venous involvement.
- Ultrasound:
- Biopsy Procedures:
- Percutaneous Needle Biopsy:
- Obtains tissue for histological confirmation.
- Considerations:
- Not always necessary if imaging is characteristic.
- Risk of bleeding, tumor seeding is minimal.
- Percutaneous Needle Biopsy:
- Staging:
- TNM Classification:
- Tumor (T): Size and extent within the kidney.
- Nodes (N): Lymph node involvement.
- Metastasis (M): Presence of distant spread.
- TNM Classification:
- Additional Tests:
- Bone Scan:
- Considers tumor size, liver function, performance status.
- Positron Emission Tomography (PET) Scan:
- Tumor size, lymph node involvement, metastasis.
- Bone Scan:
Stages
Types of Treatment
Treatment Modalities
Surgery:
- Radical Nephrectomy:
- Indications: Large tumors, central location, or when partial nephrectomy is not feasible.
- Procedure: Removal of the entire kidney, adrenal gland, and surrounding tissue.
- Side Effects: Risk of chronic kidney disease, bleeding, infection.
- Partial Nephrectomy:
- Indications: Small tumors (<7 cm), solitary kidney, bilateral tumors.
- Procedure: Removal of the tumor while preserving healthy kidney tissue.
- Side Effects: Similar to radical nephrectomy but preserves renal function.
- Minimally Invasive Techniques:
- Laparoscopic or Robotic Surgery:
- Advantages: Less pain, shorter hospital stay, quicker recovery.
- Outcomes: Comparable oncological control to open surgery.
- Laparoscopic or Robotic Surgery:
Ablative Therapies:
- Cryoablation:
- Mechanism: Freezes and destroys tumor cells.
- Indications: Small tumors, patients unfit for surgery.
- Side Effects: Bleeding, damage to surrounding tissues.
- Radiofrequency Ablation (RFA):
- Mechanism: Uses heat to destroy cancer cells.
- Indications: Similar to cryoablation.
- Side Effects: Pain, risk of incomplete ablation.
Targeted Therapy:
- Tyrosine Kinase Inhibitors (TKIs):
- Agents: Sunitinib, Pazopanib, Axitinib, Cabozantinib.
- Mechanism: Inhibit angiogenesis by targeting VEGF receptors.
- Side Effects: Hypertension, hand-foot syndrome, diarrhea.
- Efficacy: Improved PFS and OS in advanced RCC.
- mTOR Inhibitors:
- Agents: Everolimus, Temsirolimus.
- Mechanism: Inhibit mTOR pathway affecting cell growth and proliferation.
- Side Effects: Stomatitis, rash, immunosuppression.
- Efficacy: Benefit in specific patient populations.
Immunotherapy:
- Immune Checkpoint Inhibitors:
- Agents: Nivolumab (PD-1 inhibitor), Ipilimumab (CTLA-4 inhibitor), Pembrolizumab.
- Mechanism: Enhance the immune system’s ability to attack cancer cells.
- Side Effects: Immune-related adverse events (colitis, hepatitis, pneumonitis).
- Efficacy: Improved OS and ORR, especially in combination therapies.
- Combination Therapies:
- Nivolumab + Ipilimumab:
- Indications: First-line treatment for intermediate and poor-risk patients.
- Outcomes: Higher response rates and longer survival.
- Pembrolizumab + Axitinib:
- Indications: First-line treatment for advanced RCC.
- Outcomes: Improved OS and PFS compared to Sunitinib.
- Nivolumab + Ipilimumab:
Radiation Therapy:
- Usage:
- Limited role due to RCC’s resistance.
- Used for palliation of symptoms from metastatic sites.
Evidence-Based Comparisons
| Treatment | Mechanism | Side Effects | Efficacy (Survival Rate) | Study/Trial |
|---|---|---|---|---|
| Sunitinib | TKI inhibiting VEGF receptors | Hypertension, fatigue, diarrhea | Median PFS ~11 months | Motzer et al., 2007 |
| Nivolumab + Ipilimumab | PD-1 and CTLA-4 checkpoint inhibitors | Immune-mediated reactions | 18-month OS rate: 75% (intermediate/poor-risk) | CheckMate 214, 2018 |
| Pembrolizumab + Axitinib | PD-1 inhibitor + TKI | Hypertension, diarrhea, liver enzyme elevations | 12-month OS rate: 89.9% | KEYNOTE-426, 2019 |
| Cabozantinib | TKI targeting VEGFR, MET, AXL | Diarrhea, fatigue, hand-foot syndrome | Median PFS ~8.6 months (first-line, intermediate/poor-risk) | CABOSUN Trial, 2017 |
Key Studies:
- CheckMate 214 (2018):
- Findings: Sorafenib improved median OS by nearly 3 months over placebo.
- Clinical Significance: First systemic therapy approved for advanced HCC.
- KEYNOTE 426 (2019):
- Findings: Atezolizumab plus Bevacizumab significantly improved OS and PFS compared to Sorafenib.
- Clinical Significance: Established a new standard of care for first-line therapy.
Additional Resources
- Patient Advocacy Groups:
- Key Opinion Leaders:
- Dr. Robert J. Motzer: Expert in RCC clinical trials.
- Dr. Toni K. Choueiri: Leader in RCC research and treatment strategies.
- Clinical Trials:
- ClinicalTrials.gov: Database for ongoing RCC studies.
- National Cancer Institute Trials
- PubMed
- WCRF
- Image sources:
Key Findings
- Rising Incidence of Kidney Cancer: Emphasizes the need for awareness and research.
- Advancements in Treatment: Immunotherapy and targeted therapies have significantly improved survival rates in advanced RCC.
- Importance of Risk Factor Modification: Lifestyle changes can potentially reduce the risk of developing kidney cancer.
- Lack of Effective Screening Methods: Highlights the necessity for developing reliable early detection strategies.
- Personalized Medicine: Tailoring treatment based on individual patient profiles enhances outcomes.
Discussion
The increasing incidence of kidney cancer globally is a significant public health concern. While improved imaging techniques have led to more incidental findings and earlier diagnoses, the lack of effective screening methods for the general population remains a challenge. The identification of modifiable risk factors such as smoking, obesity, and hypertension underscores the importance of preventive strategies.
Advancements in treatment, particularly the development of immunotherapies and targeted therapies, have revolutionized the management of advanced RCC. Combination therapies have set new standards of care, offering improved survival rates and quality of life. However, the optimal sequencing and selection of therapies require further research, especially considering the heterogeneity of RCC.
The role of biomarkers in predicting treatment response is a critical area of investigation. While PD-L1 expression has shown some predictive value, inconsistencies across studies highlight the need for more reliable markers. Personalized medicine approaches, including genomic profiling, hold promise for optimizing treatment strategies.
Addressing the cost and accessibility of new therapies is essential to ensure equitable patient care. Multidisciplinary collaboration among healthcare providers can enhance treatment planning and support patient outcomes.
Final Recommendations
Clinical Recommendations:
- Promote Awareness of Risk Factors:
- Encourage smoking cessation programs.
- Advocate for healthy lifestyle choices to manage obesity and hypertension.
- Implement Personalized Treatment Plans:
- Utilize genomic and molecular profiling to guide therapy selection.
- Consider patient risk stratification when choosing treatment modalities.
- Enhance Multidisciplinary Care:
- Foster collaboration among urologists, oncologists, radiologists, and pathologists.
Research Directions:
- Develop Reliable Biomarkers:
- Focus on identifying markers for early detection and predicting treatment response.
- Investigate Resistance Mechanisms:
- Study how tumors develop resistance to immunotherapies and targeted agents to improve long-term outcomes.
- Explore Novel Therapies:
- Continue clinical trials assessing new drugs and combination regimens.
Policy Suggestions:
- Increase Access to Advanced Therapies:
- Advocate for healthcare policies that make treatments affordable and accessible.
- Support Preventive Health Initiatives:
- Fund programs promoting lifestyle modifications and education on kidney cancer risks.
Disclaimer
The information provided in this article is intended for general informational purposes only and should not be construed as medical advice. While every effort has been made to ensure the accuracy of the information presented, it is not a substitute for professional medical guidance, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions you may have regarding a medical condition, including kidney cancer. Do not disregard or delay seeking professional medical advice based on information found in this article. The authors and publishers are not responsible for any consequences resulting from the use of the information provided.
