Book Appointment Now

Linear Particle Accelerators (Linacs): A Cornerstone in Modern Cancer Treatment
Introduction
Cancer remains one of the leading causes of death worldwide, but advances in technology have significantly improved treatment outcomes. Linear Particle Accelerators, commonly known as Linacs, play a pivotal role in modern radiation therapy by delivering high-energy beams precisely to cancerous tumors while sparing surrounding healthy tissue. Over the years, Linacs have evolved to become more accurate and efficient, making them indispensable tools in the fight against cancer.

Detailed Description
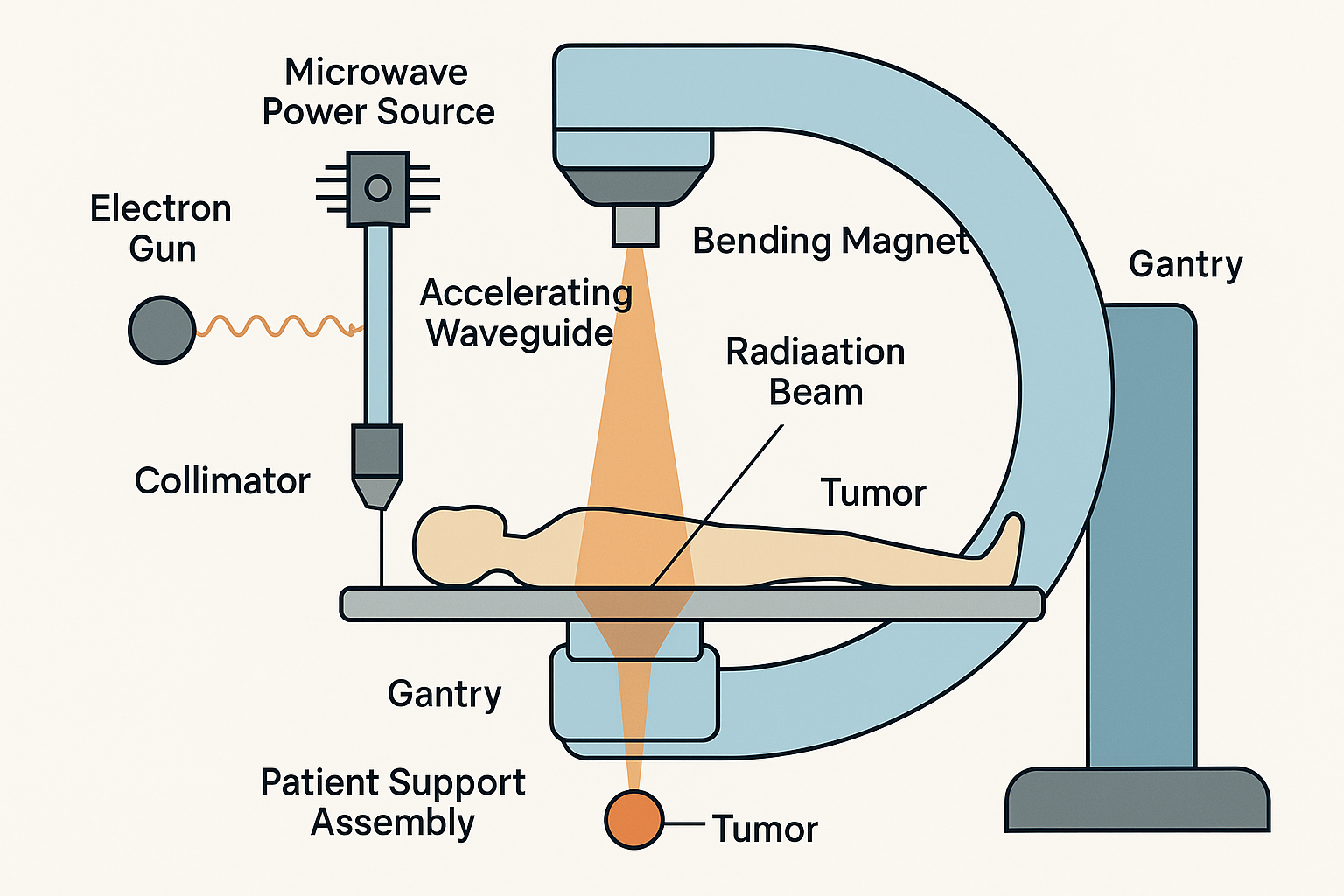
A Linear Particle Accelerator (Linac) is a sophisticated machine used to generate high-energy X-rays or electrons for radiation therapy. It accelerates electrons through a linear tube—hence the name “linear accelerator”—and directs them to produce a radiation beam that conforms to the shape of the tumor.
Key Components:
- Electron Gun: Generates electrons that will be accelerated.
- Accelerating Waveguide: A vacuum tube where electrons gain energy by passing through electromagnetic fields.
- Microwave Power Source: Devices like klystrons or magnetrons that produce microwaves used for acceleration.
- Bending Magnet: Directs the high-energy electrons toward the patient or target.
- Target: Converts electrons into high-energy X-rays when X-ray therapy is required.
- Collimator: Shapes the radiation beam to match the tumor’s dimensions, often using multileaf collimators (MLCs).
- Gantry: Rotates around the patient, allowing radiation to be delivered from different angles.
- Patient Support Assembly: The treatment couch that precisely positions the patient.
How It Works:
In simple terms, a Linac uses microwave technology—similar to that found in microwave ovens or radar systems—to accelerate electrons to nearly the speed of light. Here’s a step-by-step explanation:
- Electron Generation and Acceleration:
- Electron Gun: The process begins with an electron gun that emits electrons by heating a filament. This is akin to how a light bulb filament emits light when heated.
- Accelerating Waveguide: The emitted electrons enter a long, hollow tube called the accelerating waveguide, which is under a high vacuum to prevent electron collisions with air molecules.
- Microwave Acceleration: Powerful microwaves generated by klystrons or magnetrons are introduced into the waveguide. These microwaves create alternating electromagnetic fields that “push” and “pull” the electrons, accelerating them forward to speeds approaching that of light.
- Utilization of Accelerated Electrons:
- Direct Electron Therapy (for Superficial Tumors): For cancers located near the surface, such as skin cancers, the high-energy electrons can be used directly. Electrons have a limited penetration depth in tissue, making them ideal for treating superficial tumors without affecting deeper tissues.
- Conversion to High-Energy X-rays (for Deeper Tumors): For tumors situated deeper within the body, the accelerated electrons are directed onto a heavy metal target, usually made of tungsten. When the electrons collide with the target, they undergo sudden deceleration, emitting energy in the form of high-energy photons—X-rays—through a process known as bremsstrahlung radiation (German for “braking radiation”).
- Shaping and Directing the Radiation Beam:
- Beam Shaping with Collimators: The X-rays or electrons are then shaped to conform to the tumor’s three-dimensional shape using collimators. Multileaf collimators (MLCs) consist of numerous thin, movable metal leaves that can be individually adjusted to create a beam shape that matches the tumor’s outline precisely.
- Rotating Gantry for Multiple Angles: The Linac’s gantry rotates around the patient, allowing radiation to be delivered from various angles. By directing the beams from multiple directions, the Linac ensures that the maximum radiation dose converges on the tumor while minimizing exposure to surrounding healthy tissue.
- Maximizing Dose to Cancer Cells While Protecting Healthy Tissue:
- Targeted Delivery: The convergence of multiple shaped beams at the tumor site increases the radiation dose to cancer cells, enhancing the likelihood of destroying them.
- Sparing Healthy Tissue: Healthy tissues receive a significantly lower dose because they are only traversed by individual beams, not the concentrated intersection of all beams. This reduces side effects and damage to normal cells.
Scenario
Imagine shining several flashlights toward a small object in a dark room. Each flashlight represents a radiation beam. Individually, the light from each flashlight is not intense, but where all the beams overlap on the object, the light is much brighter. Similarly, the Linac directs multiple radiation beams that intersect at the tumor, delivering a potent dose there while keeping exposure to surrounding areas minimal.
Applications in Oncology
Linacs are primarily used in external beam radiation therapy for cancer treatment. They are versatile machines capable of delivering various types of radiation therapy, tailored to different cancer types and patient needs.
1. 3D Conformal Radiation Therapy (3D-CRT):
- Function: Utilizes imaging data to create a three-dimensional model of the tumor.
- Benefit: Allows radiation beams to be shaped and directed to match the exact shape of the tumor, minimizing exposure to healthy tissue.
2. Intensity-Modulated Radiation Therapy (IMRT):
- Function: Modulates the intensity of each radiation beam.
- Benefit: Delivers higher radiation doses to specific parts of the tumor while reducing exposure to nearby healthy tissue, enhancing treatment effectiveness.
3. Image-Guided Radiation Therapy (IGRT):
- Function: Incorporates imaging technologies like CT, MRI, or X-rays during each treatment session.
- Benefit: Accounts for tumor movement and changes in patient positioning, ensuring precise delivery of radiation.
4. Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiotherapy (SBRT):
- Function: Delivers very high doses of radiation with sub-millimeter accuracy over one or few sessions.
- Benefit: Often used for small tumors in the brain or body, reducing the overall treatment time and improving patient convenience.
Scenario:
Consider a patient with early-stage lung cancer. Traditional surgery may not be feasible due to the patient’s health. Using SBRT with a Linac, doctors can deliver high doses of radiation precisely to the tumor while sparing healthy lung tissue. This non-invasive approach offers a curative option with minimal side effects.
Advantages and Limitations
Advantages:
- Precision: Linacs can target tumors with high accuracy, reducing damage to healthy tissue.
- Versatility: Capable of delivering a wide range of radiation therapies customized to individual patient needs.
- Adaptability: Real-time imaging allows for adjustments during treatment, accounting for patient movement or tumor changes.
- Improved Outcomes: Enhanced precision leads to better tumor control and fewer side effects, improving patient quality of life.
Limitations:
- Cost: Linacs are expensive to purchase, install and maintain, which can limit their availability, especially in low-resource settings.
- Complexity: Operation requires a team of specialized professionals, including medical physicists, dosimetrists, radiation oncologists and therapists.
- Accessibility: Not all treatment centers have the latest Linac technology, potentially impacting the quality of care in some regions.
- Radiation Exposure: Despite precision, there is still a risk of radiation affecting nearby healthy tissues, leading to side effects.
Recent Developments and Innovations

Advancements in Linac technology have significantly enhanced their effectiveness and patient safety.
1. Volumetric Modulated Arc Therapy (VMAT):
- Feature: Delivers radiation by rotating the gantry around the patient in an arc, adjusting the beam shape and dose continuously.
- Benefit: Reduces treatment times and improves dose distribution, enhancing patient comfort.
2. Artificial Intelligence (AI) Integration:
- Feature: AI algorithms assist in treatment planning, dose calculations and adaptation.
- Benefit: Improves precision and efficiency, enabling personalized treatment plans and reducing planning time.
3. Flattening Filter-Free (FFF) Technology:
- Feature: Removes the flattening filter from the beam path, allowing for higher dose rates.
- Benefit: Decreases treatment time, reducing patient discomfort and potential for movement during therapy.
4. Adaptive Radiation Therapy:
- Feature: Continuously adapts the treatment plan based on changes in tumor size, shape or position.
- Benefit: Enhances treatment effectiveness by accounting for anatomical changes over the course of therapy.
5. Integration with Advanced Imaging Modalities:
- Feature: Combines MRI or PET imaging with Linac systems (e.g., MR-Linac).
- Benefit: Provides better visualization of tumors during treatment, improving targeting accuracy and sparing healthy tissue.
Safety and Patient Comfort
Safety Features:
- Quality Assurance Protocols: Regular calibration, safety checks and maintenance ensure the Linac operates correctly and safely.
- Built-in Safety Systems: Features like automatic beam shut-off prevent accidental overexposure to radiation.
- Regulatory Compliance: Linacs adhere to stringent safety standards set by regulatory bodies such as the FDA and international organizations.
Patient Comfort Considerations:
- Non-Invasive Treatment: Radiation therapy with Linacs is painless and does not involve incisions or anesthesia.
- Shorter Sessions: Innovations like VMAT and FFF technology reduce the time patients spend in treatment, enhancing comfort.
- Supportive Environment: Treatment rooms are designed to be calming and staff provide support to alleviate anxiety.
Addressing Patient Concerns:
Patients may have worries about radiation exposure or side effects. Healthcare providers explain that modern Linacs are designed with advanced technology to minimize risks. Detailed treatment planning and safety protocols ensure the safest possible delivery of radiation. Open communication and education help alleviate patient concerns, fostering a reassuring treatment experience.
Conclusion
Linear Particle Accelerators have revolutionized radiation therapy, offering precise, adaptable and effective cancer treatments. By accelerating electrons to near-light speeds and precisely directing radiation beams, Linacs maximize the dose to cancer cells while protecting healthy tissue. Technological advancements, such as AI integration and advanced imaging, continue to enhance their capabilities.
Looking ahead, Linacs are expected to become even more sophisticated, incorporating real-time tumor tracking and further personalization of treatment plans. They remain critical in oncology, providing hope and improved quality of life for cancer patients worldwide. As technology advances, Linacs will continue to be at the forefront of cancer care, embodying the fusion of innovative science and compassionate treatment.
References
- American Society for Radiation Oncology (ASTRO). (2023). Radiation Therapy for Cancer.
- National Cancer Institute. (2023). Radiation Therapy and You: Support for People With Cancer.
- Radiological Society of North America (RSNA). (2023). Linear Accelerator – Radiation Therapy.
For more information on cancer care and advancements in oncology equipment, visit CancersHub.com.



