Book Appointment Now

MRI in Oncology: Unveiling Cancer with Magnetic Resonance Imaging
Introduction
Cancer diagnosis and treatment have significantly evolved with advancements in medical imaging technology. Magnetic Resonance Imaging (MRI) stands out as a powerful, non-invasive tool that provides detailed images of the body’s internal structures. In oncology, MRI plays a crucial role in detecting, diagnosing, staging, and monitoring various types of cancer. Recent innovations have enhanced its precision and expanded its applications, making MRI an indispensable asset in modern cancer care.

Detailed Description
MRI is a medical imaging technique that uses strong magnetic fields and radio waves to generate detailed images of organs, tissues and other internal structures. Unlike X-rays or CT scans, MRI does not use ionizing radiation, making it a safer option for repeated imaging.
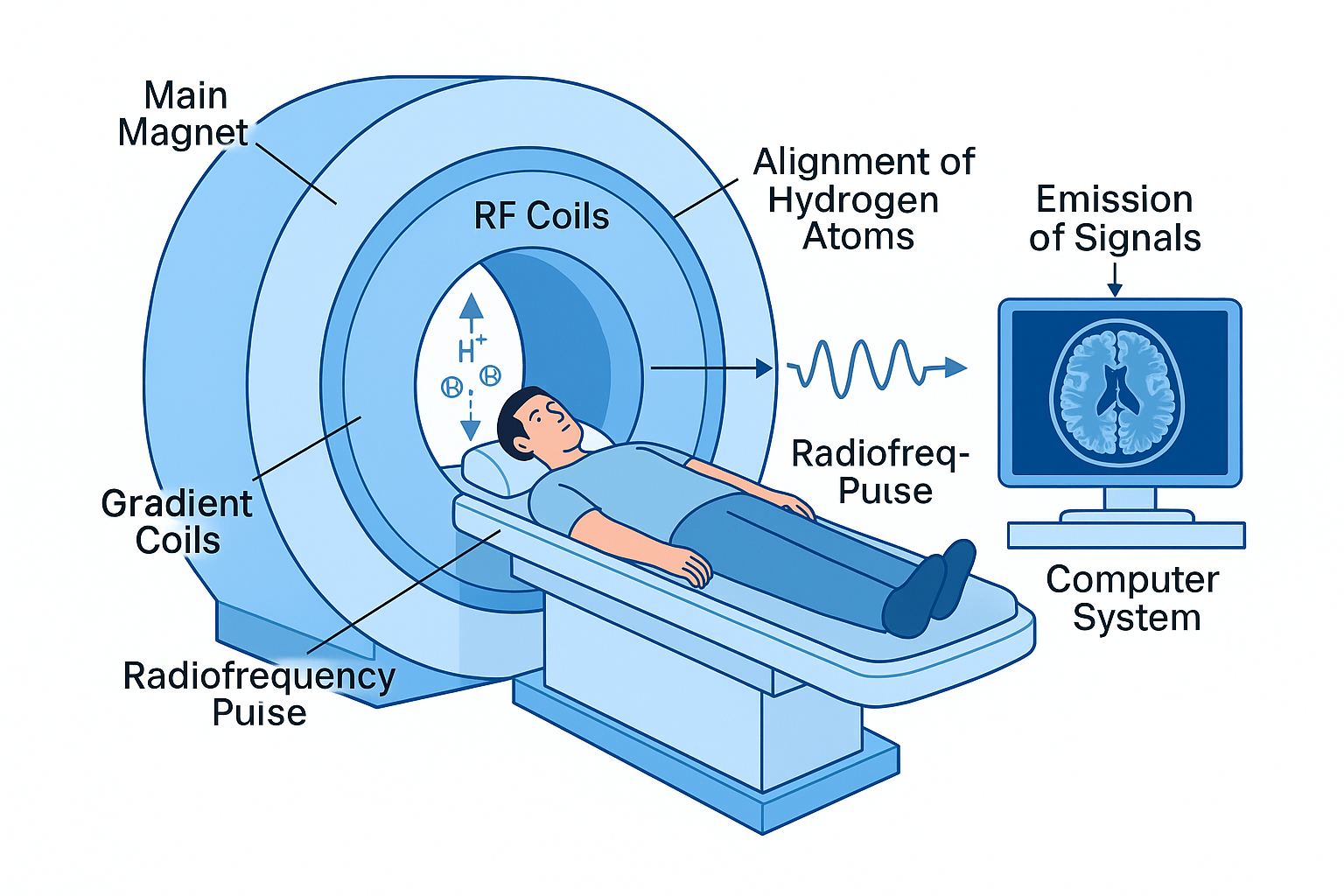
Key Components:
- Magnet: The core component that produces a strong, uniform magnetic field.
- Gradient Coils: Smaller magnets that adjust the main magnetic field, allowing for spatial encoding of the MRI signals.
- Radiofrequency (RF) Coils: Transmit radio waves into the body and receive the signals emitted by hydrogen atoms in the tissues.
- Computer System: Processes the signals to construct detailed images.
- Patient Table: Moves the patient into the bore (opening) of the MRI scanner.
How It Works:
In simple terms, the human body is largely composed of water molecules, which contain hydrogen atoms. When a patient is placed inside the MRI scanner:
- Alignment of Hydrogen Atoms: The strong magnetic field causes the protons in hydrogen atoms to align along the field’s direction.
- Radiofrequency Pulse: An RF pulse is applied, knocking the protons out of alignment.
- Signal Emission: When the RF pulse is turned off, the protons realign with the magnetic field, releasing energy in the form of radio waves.
- Signal Detection: The RF coils detect these emitted signals.
- Image Construction: The computer processes the signals to create detailed images based on the differences in signal intensity from various tissues.
Think of it like tuning a radio station; the MRI machine “listens” to signals from the body’s hydrogen atoms to create images.
Applications in Oncology
MRI has a wide range of applications in cancer care due to its excellent soft-tissue contrast and ability to image in multiple planes without repositioning the patient.
1. Detection and Diagnosis
- Identifying Tumors: MRI is highly effective in detecting tumors in soft tissues, such as the brain, spinal cord, liver, breasts, and prostate.
- Characterizing Lesions: Helps differentiate between benign and malignant masses by analyzing tissue composition.
Example Scenario:
A patient presents with neurological symptoms like headaches and vision changes. An MRI of the brain reveals a mass in the temporal lobe. The detailed images help neurologists determine that the mass is likely a glioblastoma, guiding further diagnostic steps and treatment planning.
2. Staging and Treatment Planning
- Assessing Tumor Extent: MRI provides precise information about the size, location and involvement of surrounding tissues, crucial for staging cancer.
- Surgical Planning: Surgeons use MRI images to plan the removal of tumors while preserving as much healthy tissue as possible.
3. Monitoring Treatment Response
- Evaluating Efficacy: Repeated MRIs track changes in tumor size and characteristics during and after treatment.
- Detecting Recurrence: High-resolution images help identify any signs of cancer returning.
4. Functional MRI (fMRI) and Diffusion-Weighted Imaging (DWI)
- fMRI: Measures brain activity by detecting changes in blood flow, useful in planning surgeries for brain tumors to avoid critical functional areas.
- DWI: Assesses the movement of water molecules in tissue, aiding in early detection of tumors and monitoring response to therapy.
5. Magnetic Resonance Spectroscopy (MRS)
- Chemical Analysis: Provides information about the chemical composition of tissues, helping differentiate tumor types and aggressiveness.
6. Whole-Body MRI
- Metastasis Detection: Non-invasive whole-body scans detect metastatic cancer spread without radiation exposure.
Advantages and Limitations
Advantages:
- Superior Soft-Tissue Contrast: Excellent for imaging soft tissues, providing more detail than CT scans in certain areas.
- No Ionizing Radiation: Safe for repeated use, suitable for children and patients requiring multiple scans.
- Multiplanar Imaging: Can obtain images in any plane (axial, sagittal, coronal) without moving the patient.
- Functional Imaging Capabilities: Techniques like fMRI and MRS offer insights into tissue function and metabolism.
Limitations:
- Cost and Accessibility: MRI machines are expensive to purchase and maintain, potentially limiting availability.
- Longer Scan Times: Procedures can take 30-60 minutes, requiring patients to remain still, which may be challenging for some.
- Claustrophobia and Comfort: The enclosed space of traditional MRI scanners can cause discomfort or anxiety.
- Contraindications: Not suitable for patients with certain implants or devices, such as pacemakers or metal fragments, due to the strong magnetic field.
- Noise: MRI scanners can be loud during operation, requiring the use of ear protection.
Recent Developments and Innovations

1. High-Field and Ultra-High-Field MRI
- Enhanced Image Quality: Higher magnetic field strengths (3T and above) provide better resolution and faster imaging.
- Improved Diagnostic Accuracy: Allows for the detection of smaller lesions and subtle abnormalities.
2. Open and Wide-Bore MRI Systems
- Increased Comfort: Open designs reduce feelings of claustrophobia and accommodate larger patients.
- Flexible Positioning: Enables imaging in various positions, useful for certain diagnostic needs.
3. Advanced Imaging Techniques
- Diffusion Tensor Imaging (DTI): Maps neural pathways in the brain, aiding in surgical planning.
- Perfusion MRI: Measures blood flow within tissues, helping assess tumor vascularity and aggressiveness.
4. Artificial Intelligence and Machine Learning
- Automated Image Analysis: AI algorithms assist in detecting abnormalities, segmenting tumors and predicting treatment responses.
- Workflow Optimization: Enhances efficiency by automating routine tasks and improving image reconstruction.
5. MRI-Compatible Implants and Devices
- Expanded Patient Eligibility: Development of MRI-safe pacemakers and implants allows more patients to benefit from MRI imaging.
6. Hybrid Imaging Systems
- PET/MRI Scanners: Combine metabolic information from PET with anatomical detail from MRI, offering comprehensive diagnostic data.
Ongoing Research:
- Molecular Imaging: Targets specific biomarkers within tumors for earlier and more precise diagnosis.
- Hyperpolarized MRI: Enhances signal strength from specific molecules, improving the detection of cancerous changes.
Safety and Patient Comfort
Safety Features:
- Screening Protocols: Thorough patient screening for metal implants or fragments to prevent harm from the magnetic field.
- MRI-Compatible Equipment: Use of non-ferromagnetic tools and devices in the MRI suite.
- Emergency Procedures: Protocols in place to quickly remove patients in case of adverse reactions.
Patient Comfort Considerations:
- Sedation Options: For patients with anxiety or claustrophobia, mild sedation may be offered.
- Communication Systems: Two-way intercoms allow patients to communicate with technologists during the scan.
- Ear Protection and Music: Headphones or earplugs reduce noise levels; some facilities offer music for relaxation.
- Blankets and Positioning Aids: Enhance comfort during longer scan times.
Addressing Patient Concerns:
- Preparation Guidance: Clear instructions on what to expect help alleviate anxiety.
- Child-Friendly Approaches: Specialized protocols and environments make MRI scans less intimidating for pediatric patients.
Conclusion
MRI technology has revolutionized oncology by providing detailed, high-contrast images essential for accurate cancer detection, diagnosis and treatment planning. Its ability to image soft tissues without radiation exposure makes it particularly valuable in cancer care. Advancements in MRI technology continue to enhance its capabilities, from improved image quality to the integration of AI for better diagnostic accuracy.
Looking ahead, MRI is expected to play an even more significant role in personalized cancer care. Innovations such as molecular imaging and AI-driven analytics promise earlier detection and tailored treatment strategies. As MRI technology evolves, it will continue to be a cornerstone in the fight against cancer, offering hope for improved patient outcomes and quality of life.
References
- American Cancer Society. (2023). MRI for Cancer.
- Radiological Society of North America. (2023). Magnetic Resonance Imaging (MRI).
- National Cancer Institute. (2023). MRI Scans and Cancer.
For more information on cancer care and advancements in oncology equipment, visit CancersHub.com.
Feel free to explore more about MRI and other medical equipment that are transforming cancer care. Understanding these technologies can provide reassurance and empower patients and their families throughout their cancer journey.



