Book Appointment Now
The Financial Landscape of Cancer: Resources and Strategies for Managing Costs Associated with Colorectal Cancer
Introduction
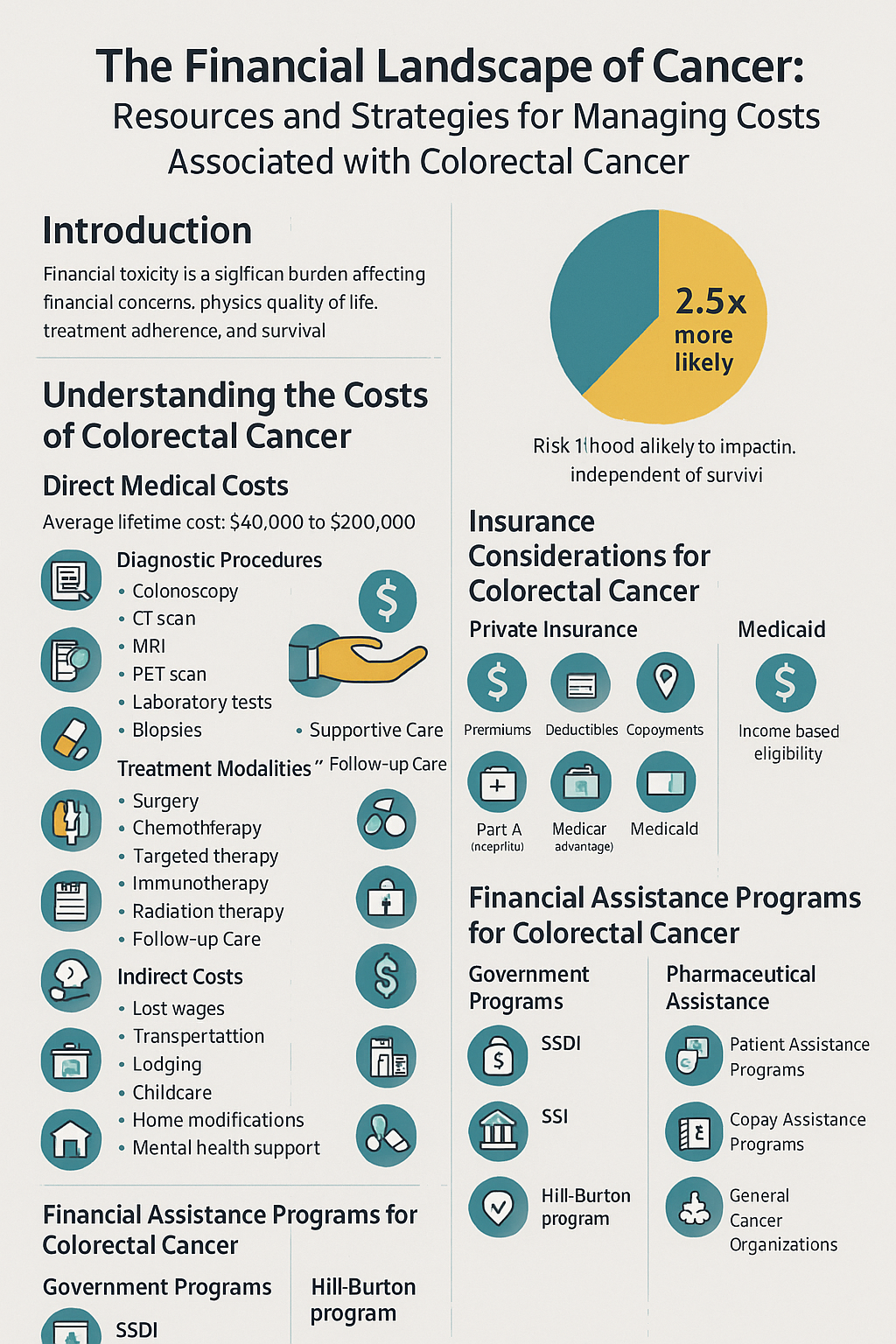
A colorectal cancer diagnosis brings numerous challenges, with financial concerns often ranking among the most overwhelming. The economic burden of cancer—frequently referred to as “financial toxicity”—can significantly impact quality of life, treatment adherence, and even clinical outcomes. Studies show that cancer patients are 2.5 times more likely to file for bankruptcy than individuals without cancer, with financial distress contributing to poorer survival rates independent of other factors.
For colorectal cancer specifically, the financial implications can be particularly significant. With treatment often involving surgery, chemotherapy, radiation, targeted therapies, and long-term surveillance, the costs accumulate quickly.
his article provides a comprehensive overview of the financial landscape of colorectal cancer and offers practical strategies for managing these expenses.
Understanding the Costs of Colorectal Cancer
Direct Medical Costs
The average lifetime cost for colorectal cancer treatment ranges from $40,000 to over $200,000, depending on stage at diagnosis, treatment approach, complications, and geographic location. These costs include:
Diagnostic Procedures
- Colonoscopy ($1,500-$3,000)
- CT scans ($500-$5,000)
- MRI ($1,000-$5,000)
- PET scans ($3,000-$6,000)
- Laboratory tests ($100-$1,000)
- Biopsies ($1,500-$2,000)
Treatment Modalities
- Surgery ($20,000-$80,000)
- Colectomy
- Low anterior resection
- Abdominoperineal resection
- Liver resection for metastases
- Chemotherapy ($5,000-$30,000 per month)
- FOLFOX regimen
- FOLFIRI regimen
- Capecitabine
- LONSURF (trifluridine and tipiracil)
- Targeted Therapies ($5,000-$15,000 per month)
- Bevacizumab (Avastin)
- Cetuximab (Erbitux)
- Panitumumab (Vectibix)
- Immunotherapy ($15,000-$30,000 per month)
- Pembrolizumab (Keytruda) for MSI-H tumors
- Radiation Therapy ($10,000-$50,000)
Supportive Care
- Antiemetics for nausea
- Growth factors for low blood counts
- Medications for pain management
- Ostomy supplies ($300-$600 monthly)
- Nutritional supplements
Follow-up Care
- Surveillance scans and bloodwork
- Office visits
- Management of long-term effects
Indirect Costs
Beyond direct medical expenses, indirect costs significantly impact the overall financial burden:
- Lost wages during treatment and recovery
- Reduced work capacity or early retirement
- Transportation to medical facilities
- Lodging during treatment away from home
- Childcare during treatment appointments
- Home modifications for recovery
- Mental health support
Research from the American Cancer Society indicates that working-age colorectal cancer survivors lose an average of $20,000 in annual wages in the years following diagnosis. For stage IV colorectal cancer, this figure can exceed $30,000 annually.
Insurance Considerations for Colorectal Cancer
Understanding Your Insurance Coverage
Private Insurance
- Premiums: Monthly costs to maintain coverage
- Deductibles: Amount you pay before insurance begins coverage
- Copayments: Fixed amount paid for specific services
- Coinsurance: Percentage of costs shared between you and insurer
- Out-of-pocket maximum: Annual limit on your cost sharing
- In-network vs. out-of-network providers: Significant cost differences
Medicare
- Part A: Hospital insurance (inpatient care)
- Part B: Medical insurance (outpatient care, doctor visits)
- Part C (Medicare Advantage): Alternative to Original Medicare
- Part D: Prescription drug coverage
- Medigap: Supplemental insurance to cover gaps in Medicare
Medicaid
- Eligibility based on income and assets
- Coverage varies by state
- Can sometimes be retroactive from date of application
Navigating Insurance Challenges
Prior Authorization
Many colorectal cancer treatments require prior authorization from insurance companies. Strategies include:
- Working with your healthcare team to complete necessary paperwork
- Following up regularly on pending authorizations
- Understanding appeal processes for denials
- Requesting expedited reviews for urgent care needs
Claim Denials
If a claim is denied:
- Request a written explanation of the denial
- Consult with your healthcare provider about resubmitting with additional information
- File a formal appeal with supporting documentation from your oncologist
- Consider external review if internal appeals are exhausted
- Contact your state insurance commissioner’s office if necessary
In-Network Care
Consider care coordination through a Cancer Center of Excellence, which may have special insurance arrangements:
- Verify network status of all providers, including: surgeons, medical oncologists, radiation oncologists, hospitals and infusion centers, radiology facilities, laboratory services
- Request “gap exceptions” when in-network specialists are unavailable
- Consider care coordination through a Cancer Center of Excellence, which may have special insurance arrangements
Financial Assistance Programs for Colorectal Cancer
Government Programs
Social Security Disability Insurance (SSDI)
- For those who have worked and paid Social Security taxes
- Colorectal cancer may qualify under Compassionate Allowance program for expedited processing
- Five-month waiting period for benefits
- Provides Medicare eligibility after 24 months of disability benefits
Supplemental Security Income (SSI)
- Need-based program for disabled individuals with limited income and resources
- Often provides immediate Medicaid eligibility
Medicare Savings Programs
- Help low-income Medicare beneficiaries with premiums and cost-sharing
- Include: Qualified Medicare Beneficiary (QMB), Specified Low-Income Medicare Beneficiary (SLMB), and Qualifying Individual (QI) programs
Veterans Benefits
- VA healthcare for eligible veterans
- Priority processing for cancer patients
- Special programs for Agent Orange exposure (associated with increased colorectal cancer risk)
Hill-Burton Program
- Free or reduced-cost care at participating hospitals
- Based on income and family size
Pharmaceutical Assistance
Patient Assistance Programs (PAPs)
- Manufacturer programs providing free or low-cost medications
- Examples specific to colorectal cancer treatments:
- Genentech Patient Foundation (bevacizumab, capecitabine)
- Merck Patient Assistance Program (pembrolizumab)
- Amgen Safety Net Foundation (panitumumab)
- Bristol Myers Squibb Patient Assistance Foundation (cetuximab)
- Taiho Oncology Patient Support (LONSURF)
Copay Assistance Programs
- Help with copayments, coinsurance, and deductibles
- Often have higher income eligibility thresholds than PAPs
- Examples:
- Patient Advocate Foundation Co-Pay Relief Program
- HealthWell Foundation Colorectal Cancer Fund
- CancerCare Co-Payment Assistance Foundation
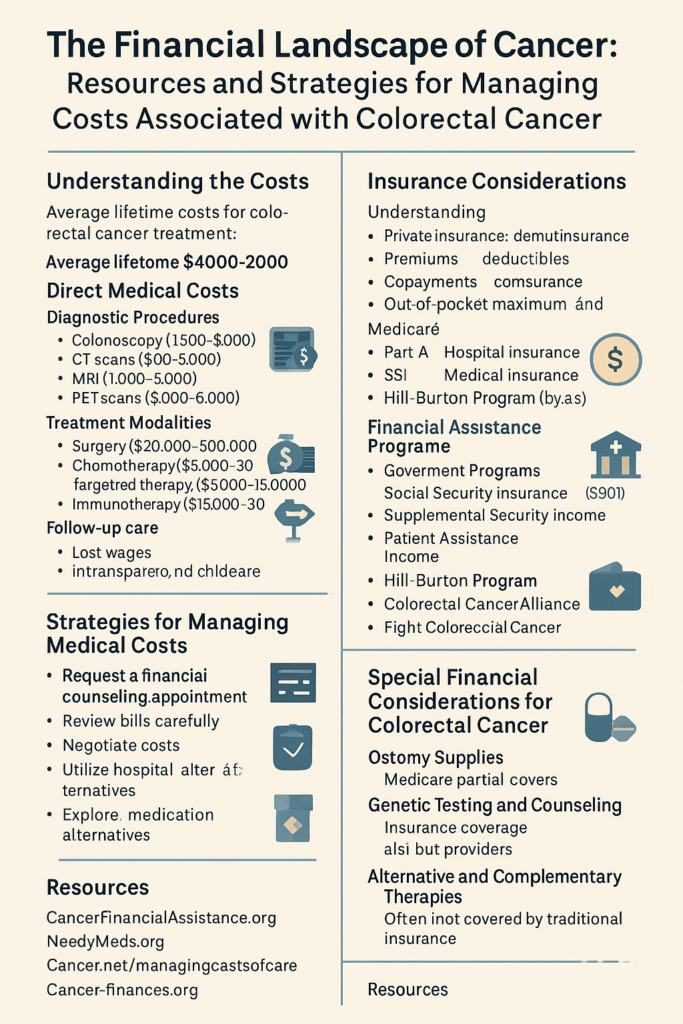
Non-Profit Organization Support
Colorectal Cancer-Specific Organizations
- Colorectal Cancer Alliance Financial Assistance Program
- Provides limited financial assistance for treatment-related costs
- Offers Blue Hope Financial Assistance for screening costs
- Fight Colorectal Cancer
- Maintains comprehensive resource guide for financial assistance
- Offers navigation services for financial concerns
- Colon Cancer Foundation
- Provides emergency financial assistance grants
- Offers navigation to other resources
General Cancer Support Organizations
- The Assistance Fund
- Disease-specific funds for medication copayments
- CancerCare
- Limited financial assistance for treatment-related expenses
- Transportation, homecare, and childcare grants
- Patient Advocate Foundation
- Case management for insurance issues
- Financial aid for expenses not covered by insurance
- American Cancer Society
- Hope Lodge for free housing during treatment
- Road to Recovery transportation program
- Patient Access Network Foundation
- Financial assistance for underinsured patients
- Disease-specific funds for colorectal cancer
Strategies for Managing Medical Costs
Before Treatment Begins
- Request a financial counseling appointment at your treatment center
- Review estimated costs for your specific treatment plan
- Identify potential financial assistance programs
- Develop payment plans if necessary
- Consider cancer centers with integrated financial navigation services
- Many major cancer centers offer dedicated financial navigators
- Can identify applicable assistance programs based on your specific situation
- Help with applications and paperwork
- Review insurance options during special enrollment periods
- Cancer diagnosis may qualify you for special enrollment outside annual periods
- Compare plans based on your expected treatment needs
- Consider maximum out-of-pocket limits and provider networks
- Ask about clinical trials
- Research-related costs typically covered by trial sponsor
- Standard of care costs usually covered by insurance
- May provide access to novel therapies at reduced cost
During Active Treatment
- Review all medical bills carefully
- Request itemized statements
- Check for duplicate charges or errors
- Compare to explanation of benefits from insurance
- Negotiate costs whenever possible
- Many hospitals offer prompt-pay discounts
- Some providers will adjust fees based on financial need
- Ask about cash pricing options
- Utilize hospital charity care programs
- Most hospitals have financial assistance policies
- Eligibility typically based on income relative to federal poverty level
- May provide retroactive coverage for recent bills
- Explore medication alternatives
- Ask about generic options when available
- Consider therapeutic alternatives that may be less expensive
- Investigate insurance formulary tiers and options
- Address problems immediately
- Don’t ignore bills you cannot pay
- Contact providers before accounts go to collections
- Document all communications regarding billing issues
Long-Term Strategies
- Take advantage of tax deductions
- Medical expenses exceeding 7.5% of adjusted gross income are deductible
- Keep detailed records of all medical expenses
- Include transportation, lodging, and meals during treatment-related travel
- Consider a Health Savings Account (HSA) if eligible
- Triple tax advantage (tax-deductible contributions, tax-free growth, tax-free withdrawals for medical expenses)
- Can be used for qualified medical expenses now or in the future
- Requires high-deductible health plan
- Review life insurance policies for living benefits
- Some policies offer accelerated death benefits for terminal illness
- Viatical settlements may provide funds from life insurance while living
- Manage employment thoughtfully
- Understand FMLA protections (12 weeks of unpaid, job-protected leave)
- Explore reasonable accommodations under ADA
- Consider implications of reduced hours on insurance eligibility
Special Financial Considerations for Colorectal Cancer
Ostomy Supplies
For patients with permanent or temporary ostomies:
- Medicare Part B covers 80% of approved amount for ostomy supplies
- Supplemental insurance may cover remaining 20%
- Check insurance limits on monthly quantity of supplies
- Explore assistance programs:
- Friends of Ostomates Worldwide
- Osto Group (discounted supplies)
- Ostomy 211 (emergency supplies)
Genetic Testing and Counseling
For hereditary colorectal cancer syndromes:
- Many insurance plans cover genetic testing when medically indicated
- Out-of-pocket costs range from $250-$5,000 depending on test complexity
- Assistance programs:
- Myriad Financial Assistance Program
- Invitae Patient Assistance Program
- Color Genomics Financial Assistance
Alternative and Complementary Therapies
- Often not covered by traditional insurance
- Consider:
- Flexible Spending Accounts (FSAs) for some eligible services
- Health Savings Accounts (HSAs) for qualified expenses
- Specialized insurance riders for complementary care
- Negotiating package rates for services
The Role of Financial Navigators
Financial navigators are professionals specifically trained to help cancer patients address financial challenges. Their services may include:
- Screening for financial assistance eligibility
- Facilitating applications for support programs
- Negotiating with providers and insurance companies
- Developing personalized financial coping strategies
- Connecting patients with resources for non-medical financial needs
Many cancer centers now employ dedicated financial navigators. If your treatment center doesn’t offer this service, organizations like the Patient Advocate Foundation and Cancer Support Community can provide similar assistance.
Addressing Employment Challenges
Legal Protections
- Americans with Disabilities Act (ADA)
- Requires employers with 15+ employees to provide reasonable accommodations
- Protects against discrimination based on medical condition
- Family and Medical Leave Act (FMLA)
- Provides up to 12 weeks of unpaid, job-protected leave
- Applies to employers with 50+ employees
- Employee must have worked 1,250 hours in previous 12 months
Workplace Accommodations
Consider requesting:
- Flexible scheduling
- Remote work options
- Modified duties during treatment
- Breaks for medication or rest
- Workspace modifications
Managing Disclosure
- No legal obligation to disclose specific diagnosis
- Strategic disclosure may help secure accommodations
- Consider working with healthcare provider on work restrictions documentation
Planning for Survivorship
Insurance Considerations
- Maintain continuous coverage
- Understand implications of changing plans with pre-existing condition
- Review coverage annually as needs change
Long-Term Financial Recovery
- Develop strategy for medical debt repayment
- Rebuild emergency savings
- Address impact on retirement planning
- Consider income protection insurance
Financial Guidance Resources
- Certified Financial Planner Board’s Consumer Advocate for Cancer
- Association of Community Cancer Centers Financial Advocacy Network
- American Cancer Society’s “Coping with Cancer in Everyday Life” resources
Conclusion
The financial impact of colorectal cancer extends well beyond the physical and emotional challenges of the disease itself. By understanding the potential costs, insurance considerations, available assistance programs, and strategic approaches to managing expenses, patients and families can reduce financial distress and focus more energy on treatment and recovery.
Remember that financial circumstances change, and assistance programs evolve regularly. Revisit your financial plan periodically, especially at transition points in care. Don’t hesitate to ask for help—financial concerns are a normal and important part of cancer management that your healthcare team should be prepared to address or refer to appropriate resources.
By taking proactive steps to address the financial aspects of colorectal cancer care, patients and families can reduce stress, improve access to necessary treatments, and potentially achieve better clinical outcomes through enhanced ability to adhere to recommended care plans.
Resources:
Financial Assistance Finder Tools
- CancerFinancialAssistance.org
- NeedyMeds.org
- Cancer.net/managingcostofcare
- Cancer-finances.org
Financial Navigation Support
- Patient Advocate Foundation: 1-800-532-5274
- CancerCare Financial Assistance Program: 1-800-813-4673
- Cancer Support Community Helpline: 1-888-793-9355
- American Cancer Society: 1-800-227-2345
Insurance Assistance
- Patient Advocate Foundation Insurance Appeals: 1-866-512-3861
- Medicare Rights Center: 1-800-333-4114
- State Health Insurance Assistance Program: www.shiphelp.org
References
- Patient Advocate Foundation. (2024). A Patient’s Guide to Navigating Financial Barriers to Care.
- Zafar SY, et al. (2023). Financial Toxicity, Material Hardship, and Mortality Among Patients With Advanced Colorectal Cancer. Journal of Clinical Oncology, 41(12), 2201-2212.
- Yabroff KR, et al. (2022). Annual Out-of-Pocket Expenditures and Financial Hardship Among Cancer Survivors Aged 18-64 Years: Analysis of the Medical Expenditure Panel Survey, 2011-2021. Journal of the National Cancer Institute, 114(6), 837-846.
- Shankaran V, et al. (2023). Cost of Care for Patients With Metastatic Colorectal Cancer in the Era of Precision Medicine. JCO Precision Oncology, 7, e2300098.
- American Cancer Society. (2024). The Costs of Cancer: Addressing Patient Costs.
- National Cancer Institute. (2024). Financial Toxicity and Cancer Treatment.
- Fight Colorectal Cancer. (2024). Financial Resource Guide for Colorectal Cancer Patients.
- Colorectal Cancer Alliance. (2024). Financial Assistance Programs for Colorectal Cancer Patients.



