Book Appointment Now
Understanding Human Papillomavirus (HPV) Infection
Introduction
Human Papillomavirus (HPV) is the most common sexually transmitted infection worldwide. Despite its prevalence, many people have limited knowledge about HPV, its potential health consequences, and available prevention methods. This article aims to provide clear, medically accurate information about HPV in an accessible way.
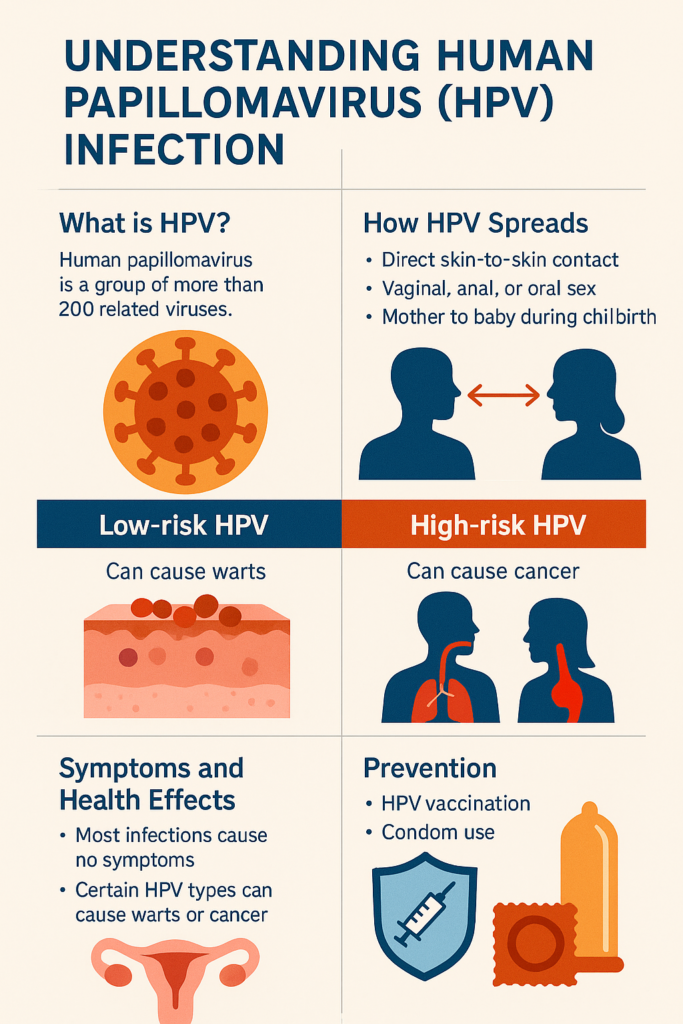
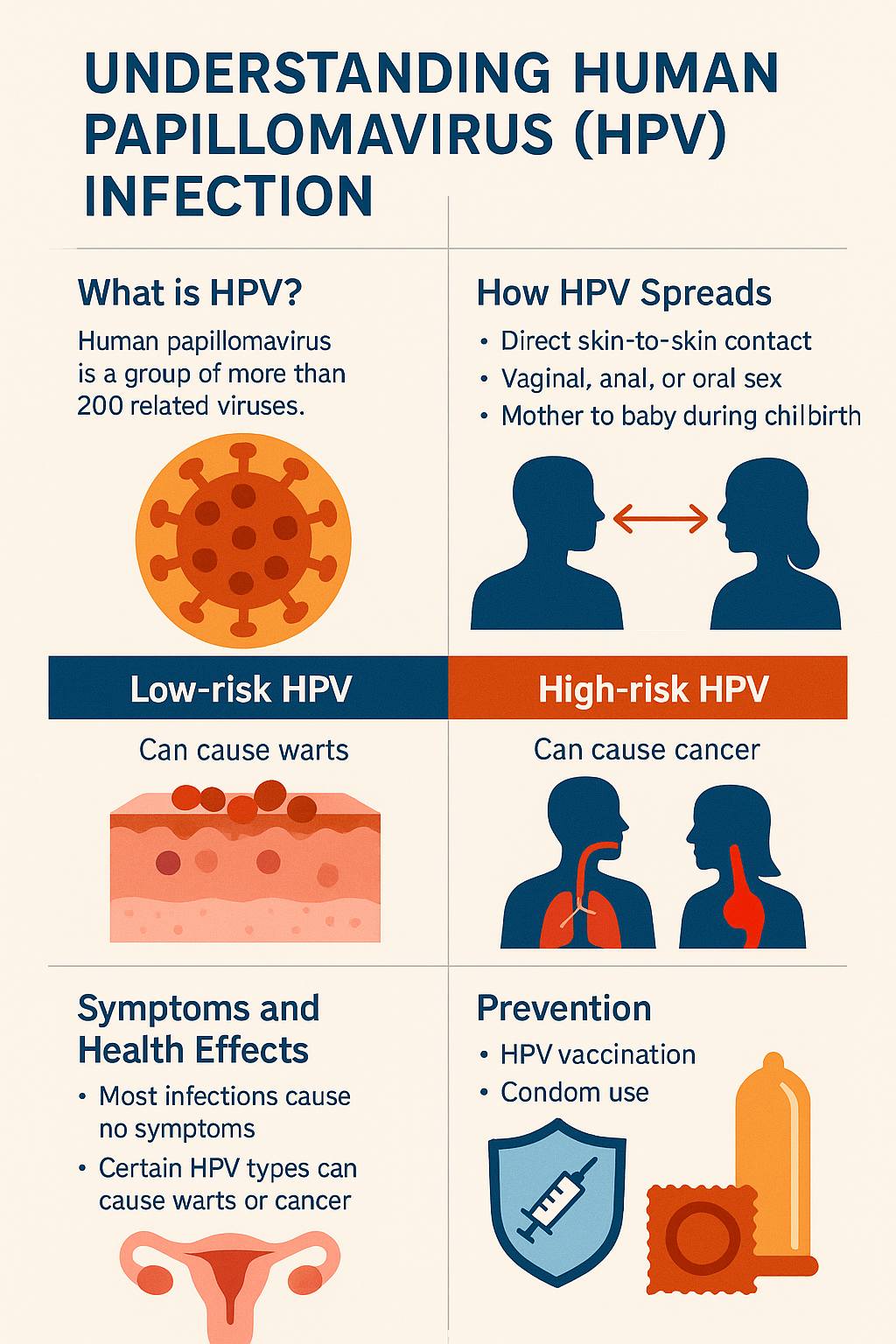
What is HPV?
Human Papillomavirus is not a single virus but a group of more than 200 related viruses. Approximately 40 of these virus types can infect the genital areas, mouth, and throat. HPV is so common that nearly all sexually active people will get at least one type of HPV at some point in their lives.
HPV viruses are categorized into two main groups:
- Low-risk HPV types (such as types 6 and 11) – These rarely cause cancer but can cause warts on the genitals, anus, mouth, or throat.
- High-risk HPV types (such as types 16 and 18) – These can cause several types of cancer, including cervical, anal, penile, vaginal, vulvar, and oropharyngeal (back of the throat, including the base of the tongue and tonsils) cancers.
How HPV Spreads
HPV spreads primarily through:
- Direct skin-to-skin contact during vaginal, anal, or oral sex
- Close intimate contact with an infected person
- Rarely, from mother to baby during childbirth
Important facts about transmission:
- HPV can spread even without symptoms – People with HPV often don’t know they’re infected because they have no visible signs
- Condoms provide partial protection but don’t completely prevent transmission since HPV can infect areas not covered by condoms
- You can be exposed to multiple types of HPV during your lifetime
Symptoms and Health Effects
Most HPV infections cause no symptoms and resolve on their own within two years. However, when HPV does cause symptoms, they vary depending on the virus type:
Low-risk HPV types may cause:
- Genital warts – Flesh-colored growths that can appear as small bumps or groups of bumps in the genital area
- Respiratory papillomatosis – Warts in the throat that can sometimes obstruct airways (rare)
High-risk HPV types:
- Usually cause no visible symptoms but can lead to cell changes that may develop into cancer over time
- Most commonly lead to cervical cancer, but can also cause other cancers mentioned earlier
- Take years or decades to progress from infection to cancer (if they do progress)
Who Is at Risk?
While anyone who is sexually active can get HPV, certain factors increase risk:
- Having multiple sexual partners
- Having sex with a partner who has had multiple partners
- Having a weakened immune system (due to HIV/AIDS or immunosuppressive medications)
- Beginning sexual activity at a young age
- Not getting vaccinated against HPV
Testing and Diagnosis
There is no single test to detect all types of HPV infection. Testing options include:
For women:
- Pap tests (Pap smears) – Detect abnormal cell changes in the cervix that might be caused by high-risk HPV
- HPV DNA tests – Specifically detect high-risk types of HPV in cervical cells
- Current guidelines recommend co-testing (both Pap and HPV testing) for women aged 30-65
For men:
- No FDA-approved test to detect HPV in men
- Visual examination may identify genital warts
- Anal Pap tests may be recommended for men at higher risk of anal cancer (such as men with HIV)
For both:
- Visual examination for genital warts
- Oral HPV testing is not routinely recommended but may be done in research settings
Prevention
HPV prevention strategies include:
HPV Vaccination
The HPV vaccine is highly effective at preventing infection from the most common cancer-causing HPV types. Current recommendations include:
- Routine vaccination for all children at age 11-12 (can start as early as age 9)
- Catch-up vaccination for everyone through age 26 if not adequately vaccinated earlier
- Some adults ages 27-45 may decide to get vaccinated after discussing risks with their healthcare provider
The vaccine is most effective when given before any exposure to HPV (before becoming sexually active).
Other Prevention Methods
- Regular screening (Pap tests and/or HPV tests for women)
- Limiting sexual partners
- Using condoms consistently (though not completely effective)
- Being in a mutually monogamous relationship
Treatment Options
There is no cure for the HPV virus itself, but treatments are available for the health problems HPV can cause:
For genital warts:
- Patient-applied treatments like imiquimod, podofilox, or sinecatechins
- Provider-administered treatments including cryotherapy (freezing), surgical removal, or laser treatment
For precancerous cell changes:
- Close monitoring with more frequent screening
- Loop electrosurgical excision procedure (LEEP) – Removes abnormal tissue
- Cryotherapy – Freezes abnormal cells
- Laser therapy – Uses light to destroy abnormal tissue
For HPV-related cancers:
- Standard cancer treatments including surgery, radiation, and chemotherapy
- Treatment depends on cancer type, stage, and individual factors
Living with HPV
If you’ve been diagnosed with HPV:
- Remember it’s extremely common – Most sexually active people get HPV at some point
- Follow your doctor’s recommendations for follow-up testing and treatment
- Maintain regular screening according to guidelines
- Practice safer sex to reduce transmission risk
- Don’t blame yourself or your partner – HPV can be dormant for years and it’s often impossible to determine when infection occurred
- Quit smoking if you use tobacco products, as smoking can make it harder for your body to clear HPV infections
When to See a Doctor
Consult your healthcare provider if you:
Are due for routine cervical cancer screening
Notice genital warts or unusual growths
Have abnormal Pap test results
Experience persistent, unusual symptoms in the genital area
Have questions about HPV vaccination
Conclusion
Human Papillomavirus is extremely common, but also largely preventable through vaccination and safer sex practices. Understanding HPV can help reduce stigma and encourage people to take preventive measures and get appropriate screening. Early detection of HPV-related cell changes can prevent the development of cancer and save lives.
Sources
- Centers for Disease Control and Prevention (CDC). (2022). Human Papillomavirus (HPV). https://www.cdc.gov/hpv/
- World Health Organization (WHO). (2022). Human papillomavirus (HPV) and cervical cancer. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer
- American Cancer Society. (2022). HPV and Cancer. https://www.cancer.org/cancer/risk-prevention/hpv.html
- National Cancer Institute (NCI). (2021). Human Papillomavirus (HPV) Vaccines. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet
- The American College of Obstetricians and Gynecologists (ACOG). (2021). Human Papillomavirus (HPV): Resource Overview. https://www.acog.org/womens-health/hpv
- International Agency for Research on Cancer (IARC). (2022). HPV and Cancer. https://www.iarc.who.int/
- Journal of the American Medical Association (JAMA). (2021). Updated guidelines for cervical cancer screening. JAMA, 325(14), 1399-1400.
- New England Journal of Medicine. (2020). Global burden of cancer attributable to HPV. N Engl J Med, 383(2), 142-152.