Book Appointment Now
Carcinoma of the Lung: Current Understanding and Management
Introduction
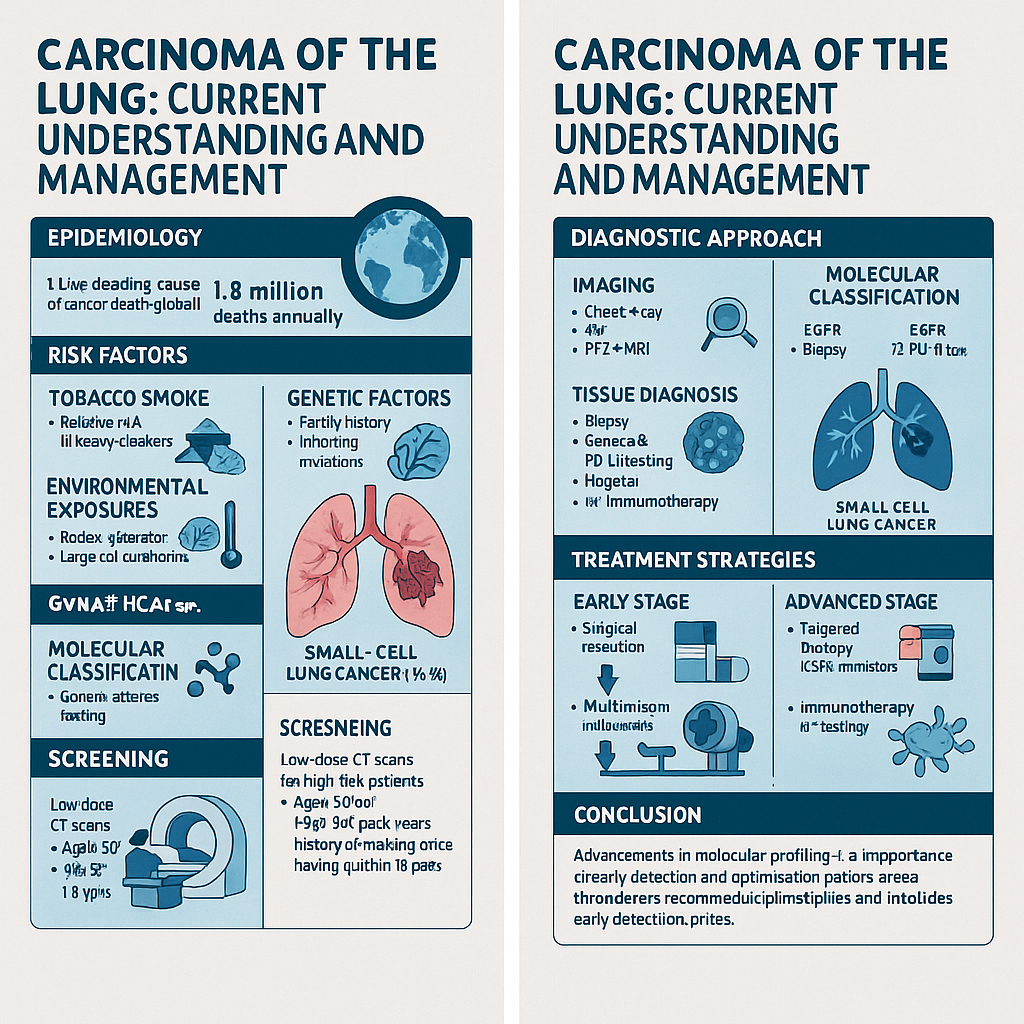
Lung cancer remains one of the most common and deadliest malignancies worldwide, accounting for approximately 1.8 million deaths annually. Despite advances in detection and treatment modalities, the overall prognosis remains challenging, with five-year survival rates varying significantly depending on stage at diagnosis and histological subtype.
This article provides an overview of the current understanding of lung carcinoma, including epidemiology, risk factors, classification, diagnostic approaches, and management strategies.
Epidemiology
Lung cancer is the leading cause of cancer-related mortality globally, with incidence rates that closely mirror smoking patterns and industrialization across different regions. While smoking rates have declined in many developed nations, lung cancer incidence among never-smokers has increased, suggesting the importance of other environmental and genetic factors.
Risk Factors
Tobacco Smoke
Cigarette smoking remains the primary risk factor, being responsible for approximately 85% of lung cancer cases. Risk correlates with cumulative exposure, quantified as pack-years, with relative risk increasing 15-30 fold in heavy smokers compared to never-smokers.
Environmental Exposures
- Radon gas (second leading cause in the United States)
- Asbestos
- Air pollution
- Occupational carcinogens (arsenic, chromium, nickel)
- Second-hand smoke
Genetic Factors
- Family history of lung cancer
- Genetic polymorphisms affecting carcinogen metabolism
- Inherited mutations in tumor suppressor genes
Histological Classification
Lung carcinomas are broadly classified into two major categories:
Non-Small Cell Lung Cancer (NSCLC)
Representing approximately 85% of cases, including:
- Adenocarcinoma (40% of all lung cancers)
- Squamous cell carcinoma (25-30%)
- Large cell carcinoma (10-15%)
Small Cell Lung Cancer (SCLC)
Comprising approximately 15% of cases, characterized by:
- Rapid growth and early metastasis
- Strong association with smoking
- Neuroendocrine features
Molecular Classification
Modern approaches to lung cancer diagnosis and treatment increasingly rely on molecular profiling:
Common Genetic Alterations in NSCLC
- EGFR mutations (10-15% in Western populations, 30-40% in Asian populations)
- ALK rearrangements (3-5%)
- ROS1 rearrangements (1-2%)
- BRAF mutations (2-4%)
- KRAS mutations (25-30%)
- MET amplification or exon 14 skipping mutations (3-4%)
- NTRK fusions (<1%)
- RET fusions (1-2%)
Clinical Presentation
Symptoms often present late in the disease course and may include:
- Persistent cough
- Hemoptysis
- Dyspnea
- Chest pain
- Weight loss
- Fatigue
- Hoarseness (due to recurrent laryngeal nerve involvement)
- Superior vena cava syndrome
- Paraneoplastic syndromes
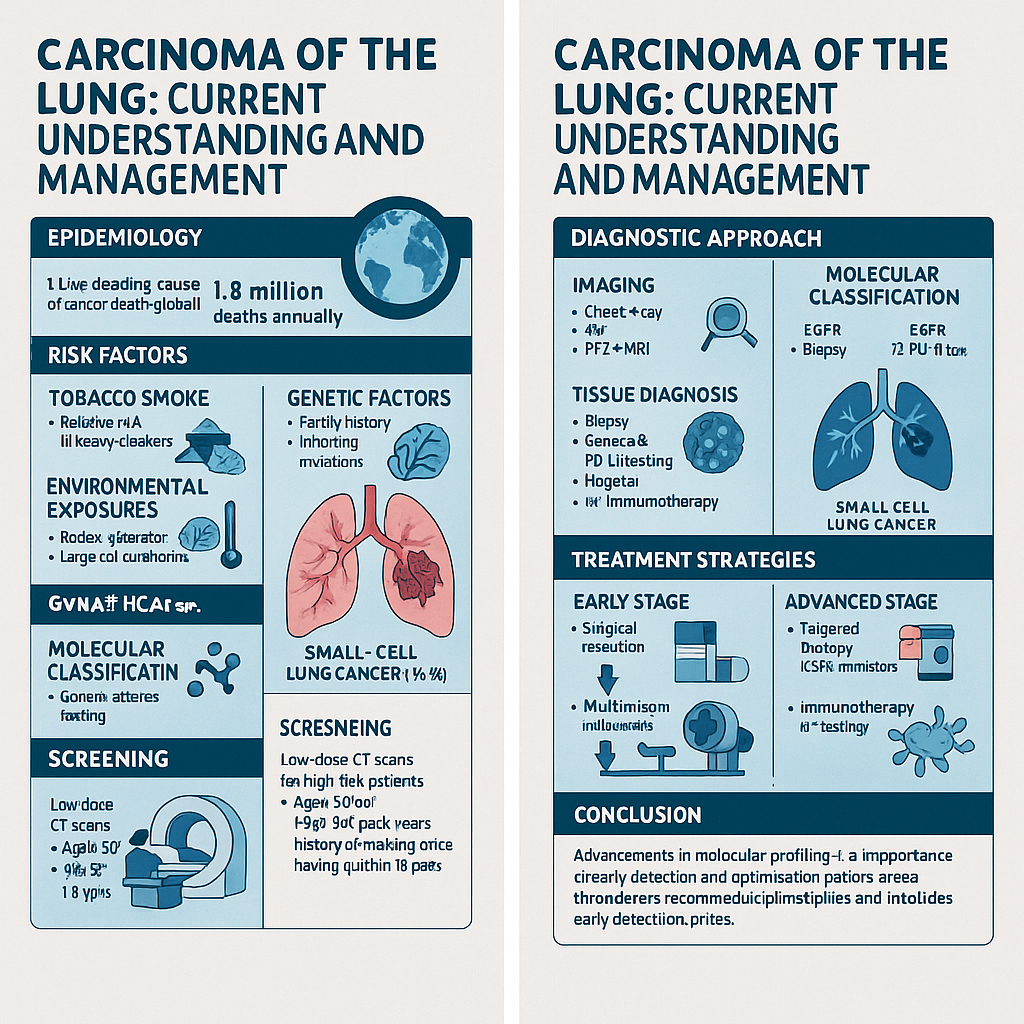
Diagnostic Approach
Imaging
- Chest radiography (initial screening)
- Computed tomography (CT) with contrast
- Positron emission tomography (PET) for staging
- Brain MRI for metastatic evaluation
Tissue Diagnosis
- Bronchoscopy with biopsy
- CT-guided percutaneous needle biopsy
- Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA)
- Mediastinoscopy
- Video-assisted thoracoscopic surgery (VATS)
Molecular Testing
- Next-generation sequencing panels
- Immunohistochemistry
- Fluorescence in situ hybridization (FISH)
- Liquid biopsy (circulating tumor DNA)
Staging
NSCLC staging follows the TNM (Tumor, Node, Metastasis) system established by the American Joint Committee on Cancer (AJCC), currently in its 8th edition. SCLC has traditionally been staged as limited or extensive disease, though the TNM system is increasingly applied to SCLC as well.
Treatment Strategies
Non-Small Cell Lung Cancer
Early Stage (I-II)
- Surgical resection (lobectomy preferred)
- Stereotactic body radiation therapy (SBRT) for medically inoperable patients
- Adjuvant chemotherapy for stage II and select stage IB
Locally Advanced (Stage III)
- Multimodality approach
- Concurrent chemoradiotherapy
- Consolidation immunotherapy (durvalumab) for unresectable stage III
- Neoadjuvant therapy followed by surgery in select cases
Advanced/Metastatic (Stage IV)
- Targeted therapy based on molecular profile
- EGFR tyrosine kinase inhibitors (osimertinib, gefitinib, erlotinib)
- ALK inhibitors (alectinib, brigatinib, lorlatinib)
- ROS1 inhibitors (entrectinib, crizotinib)
- BRAF/MEK inhibitors for BRAF V600E mutations
- Immunotherapy
- PD-1/PD-L1 inhibitors (pembrolizumab, nivolumab, atezolizumab, cemiplimab)
- Chemotherapy
- Platinum-based doublet therapy
- Pemetrexed-based regimens for non-squamous histology
Small Cell Lung Cancer
Limited Stage
- Concurrent chemoradiotherapy
- Prophylactic cranial irradiation in responders
Extensive Stage
- Chemotherapy (platinum/etoposide)
- Immunotherapy (atezolizumab or durvalumab) plus chemotherapy
- Second-line options: topotecan, lurbinectedin
Emerging Therapies
- Novel targeted therapies (HER2, KRAS G12C inhibitors)
- Antibody-drug conjugates
- Bi-specific antibodies
- Cellular therapies
- Combination immunotherapy approaches
- Tumor treating fields (TTFields)
Screening
Low-dose CT screening has demonstrated mortality reduction in high-risk populations. Current guidelines recommend annual screening for:
- Individuals aged 50-80 years
- 20+ pack-year smoking history
- Current smokers or those who quit within the past 15 years
Conclusion
The landscape of lung cancer diagnosis and treatment has evolved dramatically in recent decades. Advancements in molecular profiling, targeted therapies, and immunotherapy have improved outcomes for many patients. However, early detection remains critical, as does smoking cessation for prevention. The complexity of treatment decisions underscores the importance of multidisciplinary tumor boards in optimizing patient care.