Book Appointment Now
Brachytherapy Systems: Precision Radiation Therapy from Within
Introduction
Cancer treatment has advanced significantly over the years, with innovative technologies enhancing the effectiveness and precision of therapies. Brachytherapy systems represent one such advancement, offering a unique approach to radiation therapy by delivering radiation directly inside or next to the tumor. This localized treatment minimizes exposure to surrounding healthy tissues, improving patient outcomes and reducing side effects. Recent innovations have made brachytherapy more accessible and precise, solidifying its role in modern oncology.

Detailed Description
Brachytherapy, derived from the Greek word “brachy” meaning “short distance,” is a form of internal radiation therapy. Unlike external beam radiation therapy that delivers radiation from outside the body, brachytherapy involves placing radioactive sources directly into or near the tumor. This method allows for a high radiation dose to the tumor while limiting exposure to surrounding healthy tissues.
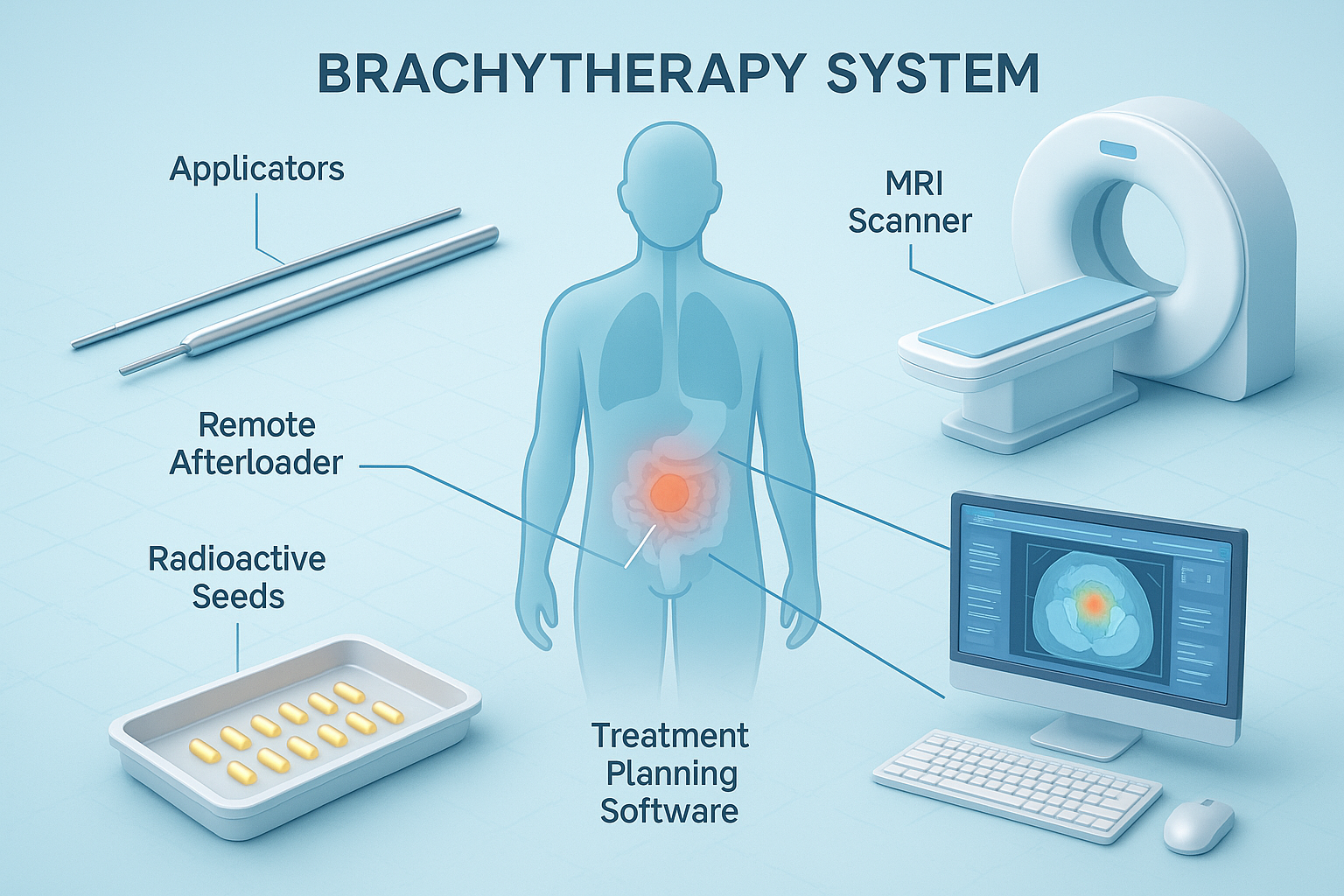
Key Components of a Brachytherapy System:
- Radioactive Sources:
- Low-Dose Rate (LDR) Sources: Emit radiation over days or weeks (e.g., iodine-125, palladium-103).
- High-Dose Rate (HDR) Sources: Deliver radiation over minutes (e.g., iridium-192).
- Temporary or Permanent Implants: Depending on the treatment plan, sources may be temporarily placed or permanently implanted.
- Applicators and Catheters:
- Devices used to accurately position radioactive sources within or near the tumor.
- Designed specifically for different body sites (e.g., needles, tubes, balloons).
- Afterloader Machines:
- Automated systems that remotely control the placement and retrieval of radioactive sources.
- Enhance safety by minimizing staff exposure to radiation.
- Treatment Planning Software:
- Advanced computer programs used to design precise treatment plans.
- Calculate optimal radiation dose distribution based on patient-specific anatomy.
- Imaging Equipment:
- Ultrasound, CT, MRI: Used for accurate placement of applicators and treatment planning.
- Real-Time Imaging: Allows for adjustments during the procedure for improved accuracy.
How Does Brachytherapy Work?
- Preparation:
- Assessment: Imaging studies determine the size, shape and location of the tumor.
- Treatment Planning: Oncologists develop a personalized plan specifying radiation dose and placement.
- Placement of Applicators:
- Anesthesia: Depending on the procedure, local or general anesthesia may be used.
- Insertion: Applicators or catheters are placed into or near the tumor using imaging guidance.
- Delivery of Radiation:
- Temporary Brachytherapy:
- HDR Brachytherapy: Radioactive sources are loaded into the applicators for short periods.
- Afterloading: The afterloader machine positions the sources according to the treatment plan.
- Permanent Brachytherapy:
- Seeds or Pellets: Small radioactive seeds are implanted and remain in the body, emitting radiation over time.
- Temporary Brachytherapy:
- Completion:
- Removal: In temporary brachytherapy, applicators and sources are removed after treatment.
- Post-Procedure Care: Patients may require monitoring and follow-up imaging.
Imagine treating a weed (tumor) in a garden without harming the surrounding flowers (healthy tissues). Brachytherapy is like placing a targeted herbicide directly on the weed, ensuring nearby plants remain unaffected.
Applications in Oncology
Brachytherapy is used to treat various cancers, either alone or in combination with other therapies like surgery and external beam radiation therapy.
1. Prostate Cancer
- Permanent Seed Implantation (LDR Brachytherapy):
- Procedure: Radioactive seeds (e.g., iodine-125) are implanted into the prostate gland.
- Benefit: Delivers continuous low-dose radiation, effective for early-stage prostate cancer.
- Example Scenario:
- A 65-year-old man with localized prostate cancer opts for LDR brachytherapy. The procedure involves implanting radioactive seeds under ultrasound guidance. Over several months, the seeds emit radiation, destroying cancer cells while preserving urinary and sexual function.
2. Gynecological Cancers (Cervical, Uterine, Vaginal)
- HDR Brachytherapy:
- Procedure: Applicators are placed in the uterus or vagina; radiation is delivered in short sessions.
- Benefit: High radiation doses target the tumor with minimal impact on nearby organs.
3. Breast Cancer
- Accelerated Partial Breast Irradiation:
- Procedure: After a lumpectomy, a balloon catheter delivers radiation to the surgical site.
- Benefit: Reduces treatment time and spares healthy breast tissue.
4. Head and Neck Cancers
- Interstitial Brachytherapy:
- Procedure: Radioactive sources are placed directly into the tumor bed.
- Benefit: Effective for cancers of the tongue, lip and oral cavity.
5. Skin Cancer
- Surface Applicators:
- Procedure: Radioactive sources are placed close to the skin’s surface.
- Benefit: Treats lesions without the need for extensive surgery.
6. Other Applications
- Esophageal, Lung, and Rectal Cancers: Brachytherapy can be used to shrink tumors obstructing passages.
- Eye Cancer (Ocular Melanoma): Plaque brachytherapy places radioactive material near the tumor.
Advantages and Limitations
Advantages:
- High Precision: Delivers a concentrated dose directly to the tumor, sparing healthy tissues.
- Shorter Treatment Times: HDR brachytherapy can reduce overall treatment duration.
- Minimized Side Effects: Lower risk of damage to surrounding organs leads to fewer complications.
- Outpatient Procedure: Many brachytherapy treatments do not require hospitalization.
- Preservation of Function: Particularly beneficial in prostate and head and neck cancers.
Limitations:
- Potential Side Effects: Includes localized pain, swelling, or risk of infection at the insertion site.
- Invasive Procedure: Insertion of applicators may cause discomfort or require anesthesia.
- Limited Applicability: Not suitable for all tumor types or locations.
- Specialized Expertise Required: Needs a skilled multidisciplinary team.
- Radiation Safety Concerns: Requires strict protocols to protect patients and staff.
Recent Developments and Innovations
1. Image-Guided Brachytherapy (IGBT)
- Integration with Advanced Imaging:
- MRI and CT Guidance: Enhances accuracy in applicator placement and dose delivery.
- Benefit: Improves treatment outcomes by targeting tumors more precisely.
2. 3D Treatment Planning Software
- Advanced Algorithms:
- Customized Dose Distribution: Tailors radiation doses to the tumor’s shape and size.
- Benefit: Maximizes tumor control while minimizing exposure to healthy tissues.
3. Robotic Brachytherapy Systems
- Automation and Precision:
- Robotic Assistance: Enhances accuracy in source placement.
- Benefit: Reduces human error and improves consistency.
4. Miniaturized Radioactive Sources
- High Specific Activity Sources:
- Smaller Implants: Allow for treatment of previously inaccessible tumors.
- Benefit: Expands the range of treatable cancers.
5. Integration with Artificial Intelligence
- AI in Treatment Planning:
- Predictive Modeling: Assists in optimizing dose distribution.
- Benefit: Enhances efficiency and personalization of therapy.
Ongoing Research:
- Radioisotope Development: Investigating new isotopes with favorable properties.
- Biodegradable Seeds: Exploring implants that dissolve after delivering radiation.
- Combination Therapies: Studying brachytherapy in conjunction with immunotherapy and chemotherapy.
Safety and Patient Comfort
Safety Features:
- Afterloader Systems: Remote loading of radioactive sources minimizes staff exposure.
- Radiation Shielding: Treatment rooms are designed to contain radiation.
- Rigorous Protocols: Adherence to safety standards set by regulatory bodies like the NRC and IAEA.
- Regular Equipment Checks: Ensures devices function correctly and safely.
Patient Comfort Considerations:
- Anesthesia Options: Use of local or general anesthesia to reduce discomfort during applicator insertion.
- Pain Management: Medications provided to manage post-procedure pain.
- Short Treatment Sessions: HDR treatments are quick, reducing time spent in the clinical setting.
- Supportive Care: Healthcare teams offer guidance and reassurance throughout the process.
Addressing Patient Concerns:
- Radiation Safety:
- Temporary Radioactivity: In HDR brachytherapy, no radioactivity remains after the procedure.
- Limited Exposure: In permanent implants, radiation levels are low and decrease over time.
- Activity Restrictions:
- Guidelines Provided: Patients receive instructions on any necessary precautions.
- Emotional Support:
- Counseling Services: Available to help patients cope with anxiety or fears related to treatment.
Conclusion
Brachytherapy systems have transformed cancer treatment by offering a highly targeted form of radiation therapy that maximizes tumor control while minimizing side effects. Their ability to deliver high doses directly to cancer cells with precision makes them critical tools in oncology. Advances in imaging, treatment planning and technology continue to enhance the effectiveness and safety of brachytherapy.
Looking forward, ongoing research and innovations promise to expand the applications of brachytherapy, making it accessible to more patients and cancer types. The integration of artificial intelligence and novel radioactive sources will further personalize treatments, improving outcomes and quality of life for cancer patients worldwide.
References
- American Brachytherapy Society. (2023). Brachytherapy Overview.
- National Cancer Institute. (2023). Radiation Therapy for Cancer.
- Radiological Society of North America. (2023). Brachytherapy.
For more information on cancer care and advancements in oncology equipment, visit CancersHub.com.
Empowering patients and healthcare professionals with knowledge about cutting-edge treatments like brachytherapy is essential in the fight against cancer. Understanding these advanced therapies can provide reassurance and support informed decision-making in cancer care.



